In this article, I briefly explain type-III hypersensitivity along with its effects.
Hypersensitivity
Hypersensitive reactions are the inflammatory reactions within the humoral or cell-mediated branches of the immune system. These reactions cause extensive tissue damage, or occasionally death. The reactions are immediate or may be delayed type depending on the symptoms.
In 1963, P.G.H. Gell and Robin Coombs categorized hypersensitive reactions into four types. The four types of reactions are named type-I, type-II, type-III, and type-IV hypersensitive reactions. Antibody or antigen-antibody complexes within the humoral branch of the immune system mediate the type-I, type-II, and type-III hypersensitive reactions. The type-IV hypersensitivity is a delayed-type hypersensitivity, which occurs within the cell-mediated branch of the immune system. It includes the delayed onset of symptoms after antigen exposure, thus called delayed-type hypersensitivity. Immediate hypersensitivity includes symptoms that manifest within minutes or hours after a sensitized recipient encounters an antigen.
Type-III hypersensitivity
When innate immune cells don’t clear antigen-antibody complexes, it leads to their accumulation, which ultimately gives rise to an inflammatory response. The reaction of antibodies with antigens generates immune complexes, and the formation of these complexes facilitates the clearance of antigens by phagocytic cells. However, sometimes, the deposition of large amounts of immune complexes can lead to tissue-damaging type-III hypersensitive reactions.
Soluble antigens give rise to type III hypersensitive reactions. When soluble antigens bind antibodies, immune complexes of different sizes form. The pathogenic potential of immune complexes is determined, in part, by their size and the amount, affinity, and isotype of the responding antibody. Larger aggregates are readily cleared from the circulation by macrophages but smaller immune complexes are not cleared easily. However, the smaller immune complexes tend to deposit in blood vessel walls, in the synovial membrane of joints, on the glomerular basement membrane of the kidney, and in the choroid plexus of the brain. The deposition of these complexes initiates a reaction that results in the recruitment of neutrophils to the site. Lytic enzymes released by the accumulated neutrophils cause tissue injury.
Immune complexes activating the complement system
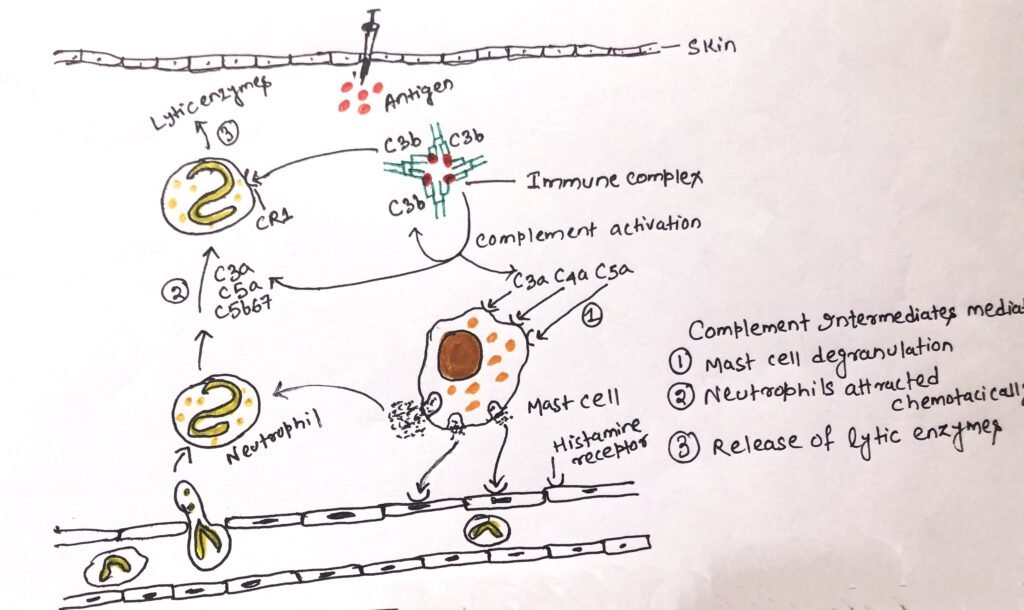
When immune complexes activate the complement system, it leads to the development of type-III hypersensitive reactions. The cleaved complement anaphylatoxins C3a, C4a, and C5a, cause localized mast cell degranulation and recruitment of inflammatory cells into the tissue, thus causing tissue damage. The chemotactic factors for neutrophils C3a, C5a, and C5b67 can accumulate in large numbers at the site of immune complex deposition (figure 1). The C3b complement component coats immune complexes and thus acts as an opsonin. A type-I complement receptor specific for C3b helps a neutrophil to bind with a C3b-coated immune complex. The complex gets deposited on the basement membrane surface, thus hindering phagocytosis. Neutrophil attempts to ingest the adhering immune complexes. However, the attempts are unsuccessful, releasing lytic enzymes. The activation of the membrane attack complex of the complement system can further mediate the destruction of tissue.
Types of type-III hypersensitivity
There may be the existence of two types of type-III hypersensitive reaction, i.e., local type or systemic type. Sensitized individuals possessing IgG antibodies against the sensitizing antigens may develop a local type III hypersensitivity reaction in the skin. When antigen is injected into the skin, circulating IgG antibodies that have diffused into the tissues form immune complexes locally. Mast cells and other leukocytes possess Fc receptors, to which immune complexes bind, thus creating a local inflammatory response with increased vascular permeability. The enhanced vascular permeability allows fluid and cells, especially polymorphonuclear leukocytes, to enter the site from the local vessels. This reaction is called an Arthus reaction (Figure 1).
The immune complexes also activate complement, releasing C5a, which attaches to C5a receptors on leukocytes. Thus, it contributes to the inflammatory reaction. This causes their activation and chemotactic attraction to the site of inflammation. The progress of the reaction causes localized tissue and vascular damage, which results in the accumulation of fluid (edema) and red blood cells (erythema) at the site. The severity of the reaction can vary from mild swelling and redness to tissue necrosis. A sensitive individual after an insect bite, may develop a rapid localized type-I reaction at the site. However, after 4-8 hours, a typical Arthus reaction also develops at the site, with pronounced erythema and edema.
A type-III systemic hypersensitivity
A type III systemic hypersensitivity reaction, also known as serum sickness, can result from the injection of large quantities of a poorly catabolized foreign antigen. Excess antigens can form small complexes, which are not easily cleared by the phagocytic cells, which can cause tissue-damaging type-III reactions at various sites. This illness was named serum sickness as it frequently followed the administration of therapeutic horse antiserum. The recipient of a foreign antiserum develops antibodies specific to the foreign serum proteins. The developed antibodies then form circulating immune complexes with the foreign serum antigens. These immune complexes fix complement and can activate leukocytes bearing Fc and complement receptors. This causes widespread tissue injury.
Serum sickness is usually a self-limiting disease, as the formation of immune complexes causes clearance of the foreign antigen. An individual begins to develop the symptoms of the illness within days or weeks after exposure to foreign serum antigens. These symptoms include fever, weakness, rashes with edema, and erythema. Urticaria is a prominent feature of the rash, implying a role for histamine derived from mast-cell degranulation. Nowadays, serum sickness is seen after the use of an immunosuppressive agent, anti-lymphocyte globulin in transplant recipients. It can also be rarely observed after the administration of streptokinase, a bacterial enzyme that is used as a thrombolytic agent to treat patients with a myocardial infarction or heart attack.
Development of other conditions
The formation of circulating immune complexes is responsible for the development of several conditions other than serum sickness. In subacute bacterial endocarditis or chronic viral hepatitis, the multiplying bacteria, or viruses are continuously generating new antigens in the presence of a persistent antibody response that fails to eliminate the organism. The disease post-streptococcal glomerulonephritis develops when circulating complexes of antibodies and streptococcal antigens are deposited in the kidneys and damage the glomeruli. Several autoimmune diseases result from circulating complexes of antibodies with self-proteins, glycoproteins, or DNA. In systemic lupus erythematosus, complexes of DNA and anti-DNA antibodies accumulate in synovial membranes, developing arthritic symptoms. When these complexes accumulate on the basement membrane of the kidney, they cause progressive kidney damage.
Some inhaled allergens provoke IgG instead of IgE antibody responses, which may be due to their excess presence in inhaled air. When a person is re-exposed to high doses of such inhaled antigens, immune complexes form in the alveolar wall of the lung. This leads to the accumulation of fluid, protein, and cells in the alveolar wall of the lung, thus ultimately slowing blood-gas interchange and compromising lung function. Continual exposure to antigens can permanently damage the alveolar membranes.
Conclusion
Hypersensitive reactions are the inflammatory reactions within the humoral or cell-mediated branches of the immune system. The four types of reactions are named type-I, type-II, type-III, and type-IV hypersensitive reactions. The deposition of large amounts of immune complexes can lead to tissue-damaging type-III hypersensitive reactions. The smaller immune complexes tend to deposit in blood vessel walls, in the synovial membrane of joints, on the glomerular basement membrane of the kidney, and in the choroid plexus of the brain.
When immune complexes activate the complement system, it leads to the development of type-III hypersensitive reactions. There may be the existence of two types of type-III hypersensitive reaction, i.e., local type or systemic type. A type III systemic hypersensitivity reaction, also known as serum sickness, can result from the injection of large quantities of a poorly catabolized foreign antigen.
The disease post-streptococcal glomerulonephritis develops when circulating complexes of antibodies and streptococcal antigens are deposited in the kidneys and damage the glomeruli. Several autoimmune diseases result from circulating complexes of antibodies with self-proteins, glycoproteins, or DNA.
You may also like:
- Type-II hypersensitivity
- The delayed-type hypersensitivity: a cell-mediated response
- Type-I hypersensitive reaction

I, Swagatika Sahu (author of this website), have done my master’s in Biotechnology. I have around fourteen years of experience in writing and believe that writing is a great way to share knowledge. I hope the articles on the website will help users in enhancing their intellect in Biotechnology.



