In this article, I briefly describe delayed-type hypersensitivity, which is a cell-mediated response.
Hypersensitivity
Our immune response gives protection to us by responding to foreign antigens. However, protecting us from foreign antigens, our immune responses can cause damage to our tissues and cells.
Multiple strategies can be applied by our immune system to reduce damage to our cells and tissues by turning off responses after the pathogen is cleared. However, these strategies can break down, which leads to disastrous immune-mediated reactions.
Failure of immune tolerance leads to some immune-mediated disorders, whereas other disorders are caused by an improperly intense innate and/or adaptive immune response to antigens, called hypersensitivities.
Delayed-Type Hypersensitivity
Hypersensitive reactions pose little or no threat to our bodies. Immunologists classify hypersensitive reactions into four categories, i.e., type-I, type-II, type-III, and type-IV hypersensitive reactions.
Some hypersensitive reactions appear immediately or within very short periods. However, some take 1 to 3 days to manifest themselves, which are known as delayed-type hypersensitivity reactions. These reactions are also known as type-IV hypersensitive reactions. These reactions result from inappropriate and excessive T-cell activation. Skin reactions to poison oak or poison ivy are examples of delayed-type hypersensitivity.
Type-IV hypersensitivity or delayed type hypersensitivity (DTH) is a completely cell-mediated response. This was first observed by the scientist Robert Koch in the year 1890.
When individuals infected with Mycobacterium tuberculosis were injected intradermally with a filtrate from mycobacterial culture, they developed a localized inflammatory response. Robert Koch named this response the tuberculin reaction. However, it was later found that this cellular response could be induced by other antigens. It was named delayed-type hypersensitivity.
This reaction is initiated by T cells. It is a delayed type of immune response, where the macrophages are recruited to surround the inflammation site. Contact dermatitis is the most common type IV hypersensitivity that occurs after exposure to Toxicodendron species, including poison oak, poison ivy, and poison sumac.
The Initiation of a Type-IV Hypersensitivity Reaction
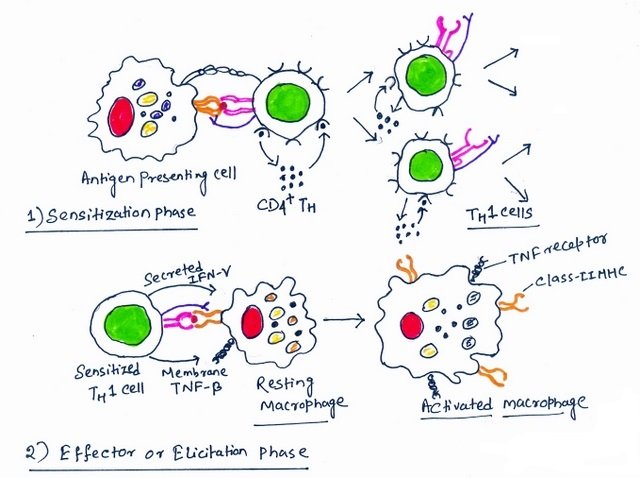
Initial sensitization by antigen is the first step of a type-IV hypersensitivity reaction or delayed-type hypersensitivity. Starting with sensitization by antigen, a DTH reaction takes 1 to 2 weeks, during which antigen-specific T cells are activated. Along with activation, these T cells attain maturity to convert into effector T cells (Figure 1).
Macrophages, dendritic cells, and dendritic cells found in the epidermis (Langerhans cells) are the antigen-presenting cells responsible for inducing a DTH response. In case of a skin reaction, these antigen-presenting cells take up antigens and carry them to regional lymph nodes. The T cells get activated in the regional lymph nodes. Generally, the sensitization phase involves the activation of TH1 CD4+ T cells. However, TH17 and CD8+ T cells can also participate in this process.
Second Exposure to a Sensitizing Antigen Leads to the Effector Phase of a DTH Response
The effector phase of the DTH response is induced by a second exposure to the sensitizing antigen. In this phase, the TH1 cells, which are previously activated, get stimulated to secrete a variety of cytokines. The secreted cytokines are interferon-γ (IFN-γ), TNF-α, and TNF-β, which help in activating macrophages and other inflammatory cells (Figure 1).
Normally, a DTH response becomes observable after 24 hours of second contact with the antigen. It peaks after 48-72 hours after this incitement. Within this stipulated period, the cytokines induce localized influx and activate macrophages. This ultimately causes the delayed onset of the DTH response. Most of the cells participating in a fully developed DTH response are macrophages and other innate immune cells, whereas only 5% of cells are antigen-specific T cells.
Role of Macrophages in a DTH Response
The cells that initiate the DTH response are TH1 cells, whereas the activated macrophages are the principal effector cells. The cytokines IFN-γ, TNF-α, and TNF-β induce blood monocytes to attach to the vascular endothelial cells and migrate from the blood into the surrounding tissues. In the surrounding tissues, they get differentiated into activated macrophages. Activated macrophages multifold the response of T helper cells by producing cytokines and recruiting more monocytes and neutrophils.
The infection area possesses elevated phagocytic activity and accumulation of lytic enzymes. This is a consequence of the activity of macrophages, which leads to non-specific destruction of cells. The bacterium Mycobacterium tuberculosis blocks the fusion of macrophage endosomes with lysosomes, thus living inside endosomes. But these blocks can be palliated by cytokines derived from T cells so that the bacteria can be killed.
Immune responses clear the target pathogens with agility and little tissue damage. However, if the antigen is not easily cleared, it leads to a prolonged DTH response. The response can be damaging for the host. This is followed by continuous activation of macrophages. This induces a close adherence among themselves, leading to an epithelioid shape. Sometimes, macrophages also fuse to form multinucleated giant cells.
The normal tissue cells are replaced by these giant cells. This leads to the formation of palpable nodules and the release of lytic enzymes, ultimately destroying the surrounding tissue. This is known as a granulomatous response, which can cause damage to the blood vessels and substantial tissue necrosis.
The Way to Detect the DTH Reaction
The DTH reaction can be detected by observing a skin lesion in an animal developed by an intradermal antigen injection. If the skin test reaction comes out to be positive, then it shows the individual has a population of sensitized TH1 cells specific for the test antigen.
To test the exposure of Mycobacterium tuberculosis, an individual is intradermally injected with purified protein derivative extracted from the cell wall of the bacterium. If the individual is previously exposed to the bacterium, then a red, slightly swollen, firm lesion is noticed at the injected site within 2-3 days.
The DTH response is mediated by TH1 T Cells
The DTH response to Mycobacterium antigens is mediated generally by TH1 T cells. However, DTH reactions can also be mediated by TH17 and CD8+ T cells. Contact dermatitis is a skin DTH response induced by the toxins found in plants in the genus Toxicodendron, e.g., in the plants’ poison oak and poison ivy. The toxin known as urushiol activates the DTH response by inducing TH1 cells, CD8+, and TH17 T cells.
The toxin urushiol, after undergoing oxidation in the body, binds covalently to skin proteins. It is picked up by skin dendritic cells and carried to the draining lymph node. There, they are degraded into peptides, presented by class-II MHC proteins, and induce the formation of TH1 cells.
The release of chemokines by these sensitized effector cells causes the recruitment of cytokines. IFN-γ, TNF-α, and leukocytes are recruited to the sites, which leads to activation of macrophages. The activated macrophages release inflammatory cytokines, lytic enzymes, reactive species, and reactive oxygen species that cause tissue damage.
Activation of CD8+ T cells
MHC class-I-bound modified peptides can activate CD8+ T cells to produce effector cytotoxic T lymphocytes. These T lymphocytes in the skin are activated by MHC class I expressed by skin cells and the urushiol-bound peptides. After activation, these cells release cytokines for macrophage activation or to decimate those skin cells. TH17 cells also generate DTH responses to urushiol.
The skin disease, severe dermatitis related to some drug reactions, is caused by CD8+ T cells and NK cells. These CD8+ T cells induce the death of keratinocytes in the skin or mucosal membrane. Stevens-Johnson syndrome, erythema multiforme, and toxic epidermal necrolysis are diseases in which this mechanism remains quite active and can be fatal. These complications are more common in males than females and typically occur in young adults.
A DTH response can be avoided by snubbing the causative antigen. After the development of hypersensitivity, the exaggerated immune response can be suppressed by topical or oral corticosteroids.
Conclusion
Hypersensitivity arises from the improper, intense innate or adaptive immune response to antigens. As the name suggests, the delayed-type hypersensitive reactions take some time to manifest themselves. The delayed-type hypersensitivity is a cell-mediated immune response.
The TH1 cells initiate the DTH responses. The activated macrophages are the principal effector cells. They multiply the response of T helper cells by producing cytokines and recruiting more monocytes and neutrophils. The DTH reactions can also be mediated by TH17 and CD8+ T cells.
You may also like:
- Contraction of our immune response and the response of effector and memory lymphocytes
- Cytokine families and their functions
- The effector cells of the immune system
- The mechanism of killing of target cells by effector cells

I, Swagatika Sahu (author of this website), have done my master’s in Biotechnology. I have around fourteen years of experience in writing and believe that writing is a great way to share knowledge. I hope the articles on the website will help users in enhancing their intellect in Biotechnology.



