In this article, I briefly describe the pre-transplantation tests necessary before organ transplantation. Transplantation success depends primarily on the immune compatibility between the donor and recipient. Because the immune system is designed to recognize and attack foreign tissues, several detailed tests are required to minimize the risk of graft rejection. These compatibility assessments form the foundation of modern transplant immunology and guide safe and effective organ transfer.
Organ transplantation
Removing an organ from one’s body and placing it in a recipient’s body to fulfill the need for a missing organ is known as organ transplantation. In the fifth century B.C., the legendary surgeon from India, Sushruta, expressed nose reconstruction for the first time. This process required the collection and transfer of skin from one site to another. Today, this type of transfer is known as an autograft and is most likely to succeed.
The Evolution and Ongoing Challenges of Organ Transplantation
Joseph Murray and colleagues in Boston, in the year 1954, first successfully transplanted a kidney between identical twins. However, tackling the obstacle of MHC molecules took nearly seven years. Dr. Samuel Kountz, an African American transplant surgeon at Stanford, along with a team of surgeons, completed the first non-twin living human transplant. In this procedure, a kidney from a mother is transplanted to her daughter. This pioneering work with immunosuppressants and a new kidney perfusion technique emerged as a new hope among physicians for the success of organ transplantation worldwide. Today, the transfer of various organs between non-identical individuals is being done with more frequency and a high success rate. However, the immediate availability of organs still becomes a scourge for the patients and the physicians as well.
Over 30,000 solid organ transplants were performed in the US in the year 2016. Though the clinical outcomes have progressed considerably, the process is facing major obstacles. Immunosuppressive drugs play a vital role in increasing the short-term survival of the transplant. However, they cause medical complications in patients. New research with new treatments that promise more specific tolerance to the transferred tissue without any hindrance to immune function is under development.
Today, advances in immunosuppressive medications and improved methods for organ retrieval and preservation have greatly reduced the challenges posed by geography and donor-recipient compatibility. Even so, three key pre-transplantation tests still need to be performed before an organ can be safely transplanted.
- Blood typing
- MHC matching
- Cross-matching
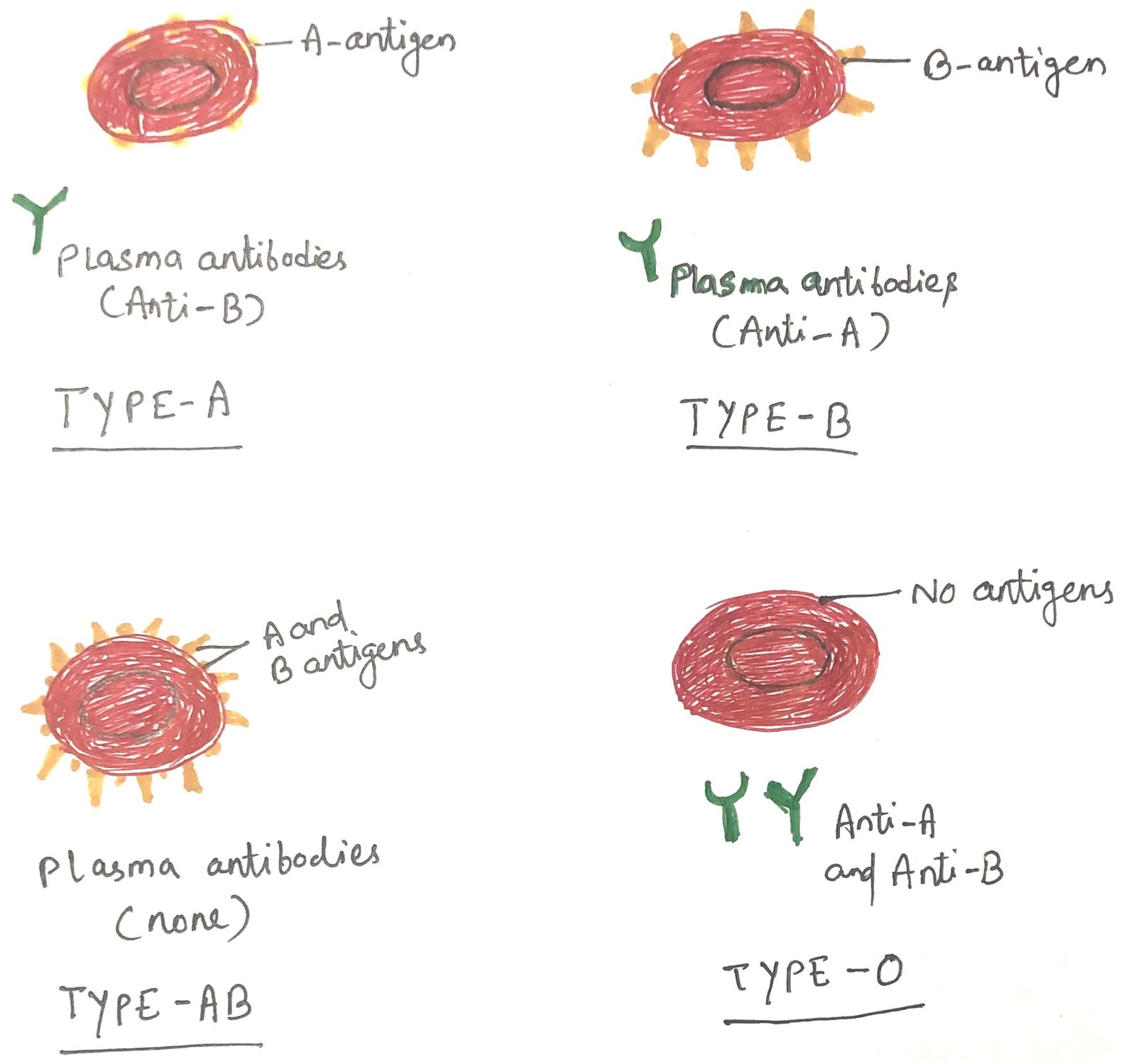
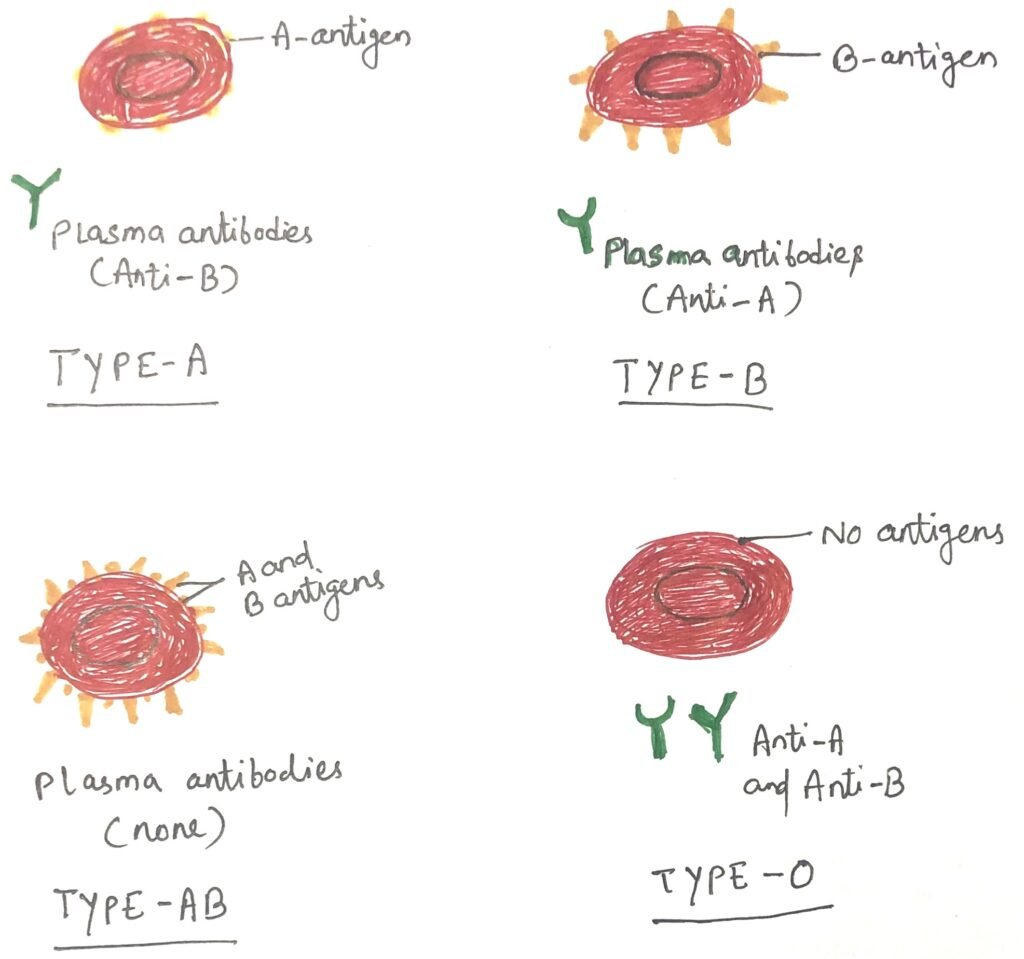
ABO Blood Group Compatibility in Transplant Rejection
The strongest graft rejection responses often arise from differences in ABO blood groups (Figure 1) between the donor and recipient. In fact, the first human kidney transplant attempt in 1933 failed for this very reason, an incompatible blood type match. ABO antigens are present not only on red blood cells but also on epithelial and endothelial cells. Thus, both donor and recipient must be carefully tested for blood group compatibility. If the recipient has antibodies against any of the donor’s ABO antigens, the transplanted organ will be rapidly destroyed through antibody-mediated lysis, a reaction known as hyperacute rejection. Therefore, most organ transplants are performed between individuals with matching ABO blood types to prevent this outcome.
MHC Matching and Its Importance in Transplantation
Assessment of MHC compatibility is a crucial step in evaluating potential organ donors for a recipient. When precise MHC matching is especially critical and a living donor is available, parents or first-degree siblings are usually preferred, followed by other close relatives. However, advancements in immunosuppression and immune tolerance strategies have made it possible for solid organ transplants to succeed even when there is substantial or complete HLA mismatch. This approach is necessary for organs such as the heart and lungs, which can survive only a few hours outside the body. Their short preservation time limits long-distance transport, making semilocal transplantation the only practical option.
In contrast, bone marrow transplantation requires the strictest MHC screening. Here, at least partial HLA compatibility is vital to ensure that the transplanted immune cells. It includes antigen-presenting cells and T cells, which can properly recognize the recipient’s MHC molecules and coordinate an effective immune response.
Serologic and molecular approaches are both used to evaluate HLA compatibility, a procedure referred to as tissue typing. The choice of method depends on the organ involved and the urgency of the results required. Molecular assays that employ sequence-specific primers to identify donor and recipient HLA alleles have become more widely used, especially in bone marrow transplants. These molecular techniques offer higher specificity and finer resolution than traditional serologic methods for identifying MHC molecules.
Role of Minor Histocompatibility Antigens in Graft Rejection
The compatibility of donor and recipient MHC molecules is not the only factor that determines whether a transplant will be accepted. Even with perfectly matched MHC antigens, a graft may still be rejected because of differences at other genetic sites, such as the minor histocompatibility loci. Alloreactive T cells can directly recognize non-self MHC molecules through their TCRs on both TH and TC cells. In contrast, minor histocompatibility antigens are detected only when their peptide fragments are presented on self MHC molecules. Although rejection driven solely by minor antigen differences is generally less severe, it can still result in graft failure. For this reason, immunosuppression is typically needed even when donor and recipient are fully HLA-matched.
Cross-Matching and the Detection of Preformed Anti-Donor Antibodies before Transplantation
Before transplantation, it is essential to check whether the recipient has any pre-existing antibodies against the donor’s alloantigens. Individuals can develop antibodies to non-self HLA proteins for various reasons. However, those who have received earlier blood transfusions or previous grafts are particularly likely to have them. This evaluation, known as cross-matching, is the most critical compatibility test conducted before solid organ transplantation. A positive cross-match indicates that the recipient already carries antibodies against the donor’s HLA molecules, making rapid rejection highly probable. Unlike ABO or MHC expression, antibody levels in a person can change over time. Someone who previously lacked antibodies to certain MHC molecules may produce them after a new exposure. For this reason, cross-matching is always carried out immediately before the transplantation procedure.
Luminex Assay for Detecting Donor-Specific Anti-HLA Antibodies
The Luminex assay uses fluorescently labeled microbeads coated with specific HLA proteins, with each protein linked to a uniquely intense fluorochrome. These HLA-coated beads are incubated with the recipient’s serum. This helps clinicians accurately identify which donor-specific anti-HLA antibodies are present before transplantation. The value of thorough cross-matching was highlighted in a landmark 1969 study. Nearly 80% of kidney transplant patients with a positive cross-match experienced immediate graft rejection, compared with only about 5% of those who tested negative.
Conclusion
Successful transplantation depends on a careful and multilayered evaluation of donor–recipient compatibility. Beyond matching ABO blood groups and assessing MHC compatibility, clinicians must also consider differences in minor histocompatibility antigens. This can still trigger rejection even when major HLA alleles are identical. The detection of preformed anti-donor antibodies through cross-matching remains one of the most critical steps, as the presence of these antibodies can lead to rapid, hyperacute rejection. Modern tools such as the Luminex assay precisely identify donor-specific anti-HLA antibodies. It greatly improves the accuracy of compatibility testing. Together, these approaches underscore how advancements in immunology and diagnostic technology have significantly strengthened transplant safety and increased the likelihood of long-term graft survival.
You may also like:
- The basics of organ transplantation
- The Expression of MHC Genes and Diversity Between Different MHC Classes
- Therapeutic Approaches to Immune Suppression
- Induction of Immune Tolerance in Organ Transplantation

I, Swagatika Sahu (author of this website), have done my master’s in Biotechnology. I have around fourteen years of experience in writing and believe that writing is a great way to share knowledge. I hope the articles on the website will help users in enhancing their intellect in Biotechnology.