In this article, I provide a brief overview of how the intestinal immune system recognizes and responds to pathogens.
Intestine and Pathogens
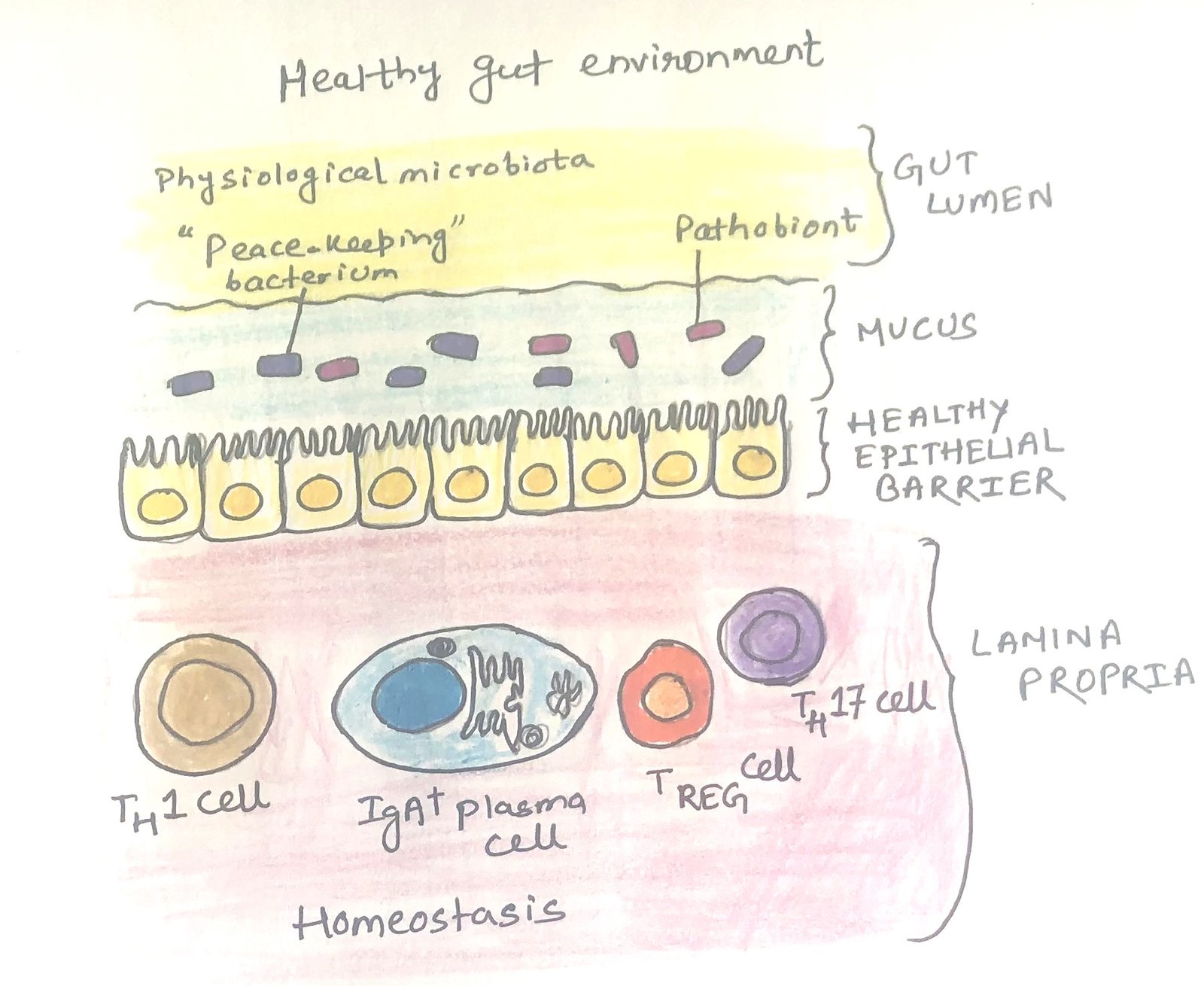
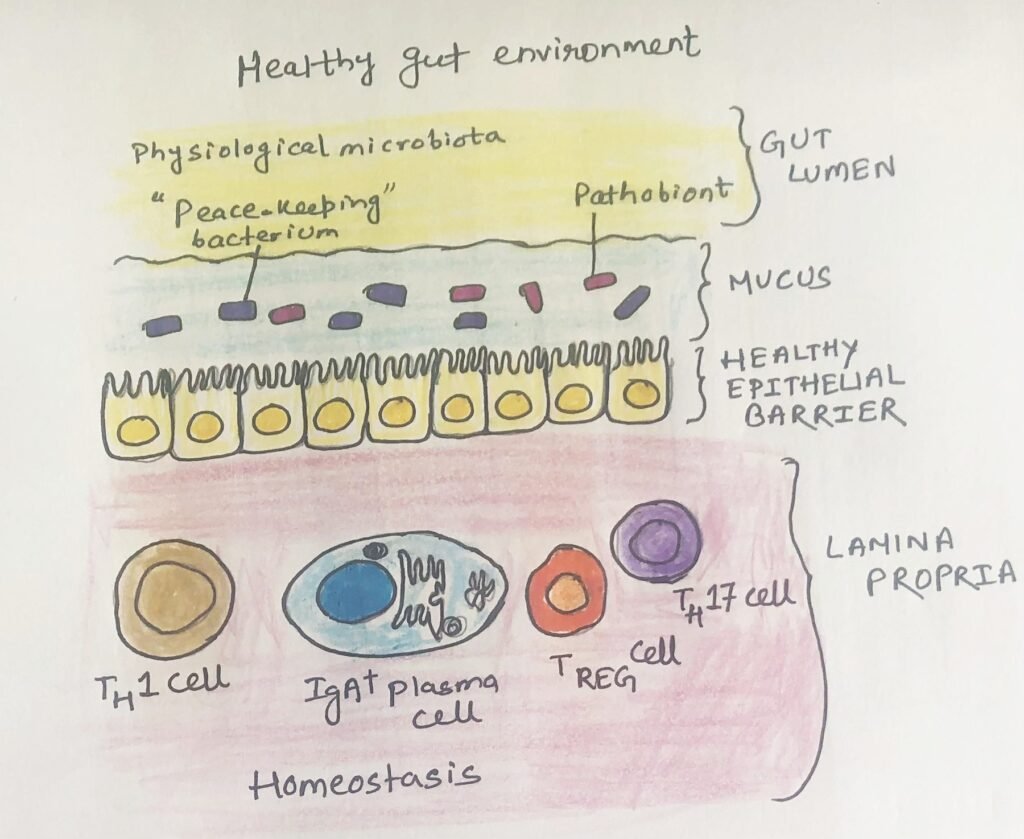
Most organisms that live in harmony with us are not harmful and help create a tolerant environment in the intestines. The gut immune system ensures a safe separation between the epithelial surfaces and even the beneficial commensal bacteria, known as pathobionts (Figure 1), which have the potential to cause disease in hosts with weakened immune systems. The most harmful microorganisms typically come from external sources. Our gut has developed various strategies to detect, respond to, and eliminate them.
The Gut Immune System and Its Response to Pathogens
Inflammation in the gut causes irritation and discomfort. However, these reactions are protective and structured to clear pathogens. Immune responses, which result in chronic inflammation, are different from these inflammatory responses.
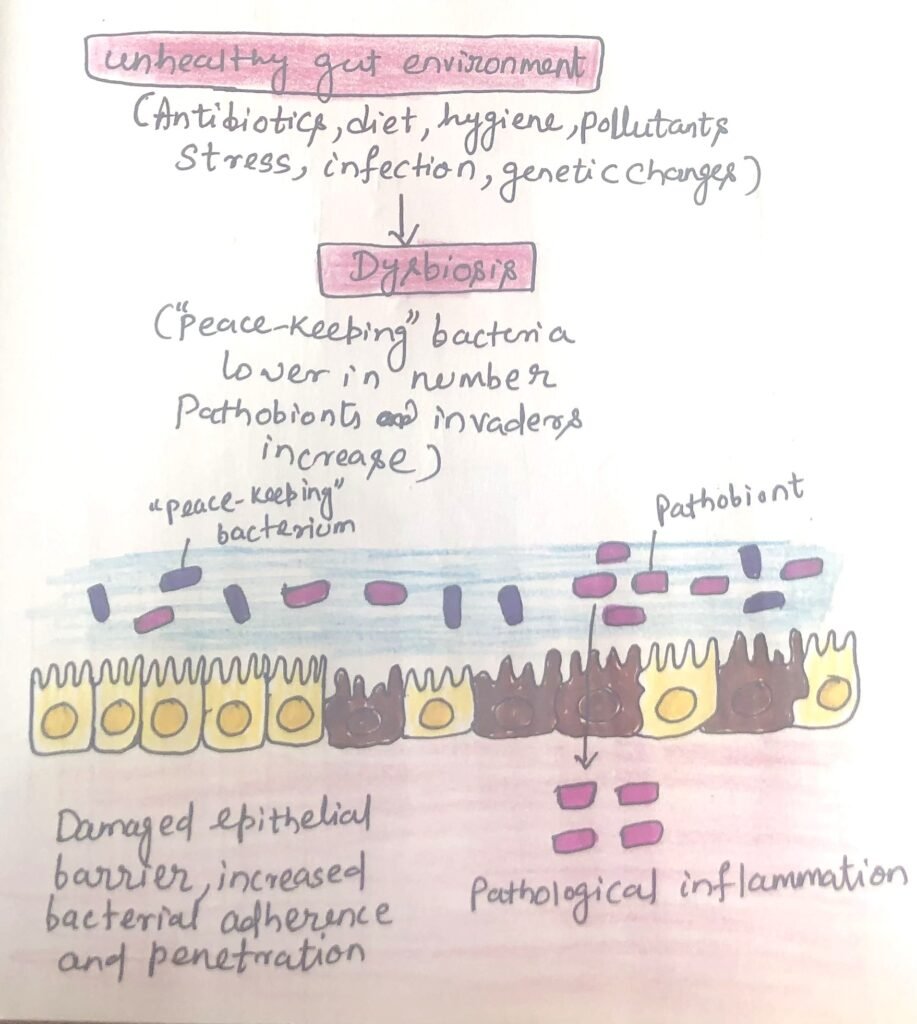
Pathogens fight with commensal bacteria for space and nutrients in the gut. Certain pathogens thrive by utilizing metabolites produced by commensal bacteria and by breaking down molecules that commensal organisms are unable to process, allowing them to exploit ecological niches that are inaccessible to commensals. Ironically, antibiotics give invading bacteria a competitive edge and improve access to the intestinal lining (Figure 2).
The two types of responses to gut pathogens can be categorized into two phases, i.e., the inductive phase and the effector phase. The response begins in the inductive phase. In the effector phase, the mature immune cells actively work to clear the pathogen and repair damage.
The inductive phase has similarities with other immune responses. It begins when epithelial cells and antigen-presenting cells, which have detected microbes through pattern recognition receptors, shift to producing pro-inflammatory signals instead of tolerogenic ones. For example, the interaction with TLR5, a receptor that detects bacterial flagellin, typically triggers inflammation. In contrast, interactions with TLR2 can promote tolerance and play a key role in resolving infections and maintaining epithelial integrity. Pathogens activating NOD-like receptors and triggering inflammatory pathways in macrophages and epithelial cells shift the immune system away from tolerogenic responses. Thus, triggering protective inflammatory reactions.
Positioning of Pathogen Recognition Receptors Provides Information to Immune Cells
The positioning of PRRs within cells helps immune cells differentiate between healthy and harmful microbial interactions. For example, TLR5 is found exclusively on the basolateral side, not the apical side, of epithelial cells in the large intestine. As a result, this receptor is only activated by bacteria when the mucosal barrier is compromised or when the bacteria become invasive.
Antigen-Presenting Cells Polarize Naïve T Cells
Activated antigen-presenting cells signal naive T cells about the presence and nature of an antigen. Instead of directing naive T cells towards the regulatory pathway, antigen-presenting cells activated by pathogens steer them towards either the TH1 and inflammatory TH17 lineages or the TH2 and TH9 lineages, depending on the type of microorganism they encounter.
The T cells and antigen-presenting cells, after encountering an antigen, spur class switching of B cells to more pro-inflammatory IgG classes instead of inducing IgA class switching. This protects the body from the spread of infection.
Activation of Type-1 and Type-2 Responses
The effector phase includes the mobilization of cells and mechanisms to eliminate or expel the invading organism, and it differs based on the type of organism involved. Activation of a type 1 response foils some bacterial infections, where inflammatory ILC3 and TH17 recruit phagocytic neutrophils. Bacterial infections can trigger ILCs to release IL-22, prompting epithelial cells to produce antimicrobial peptides that kill bacteria. In the case of worm incursion, type 2 responses are activated, involving ILC2 and TH2 cells, which then recruit eosinophils and increase mucus production and peristalsis. The muscle contractions in the intestines, known as peristalsis, aid in digestion and help thrust out the worms.
Conclusion
The gut immune system ensures a safe separation between the epithelial surfaces. Even the beneficial commensal bacteria, known as pathobionts, have the potential to cause disease in weakened hosts. Our gut has developed various strategies to detect, respond to, and eliminate them. Pathogens fight with commensal bacteria for space and nutrients in the gut.
There are two types of responses to gut pathogens. The two phases are the inductive phase and the effector phase. The inductive phase begins when epithelial cells and antigen-presenting cells detect microbes through pattern-recognition receptors.
The positioning of PRRs within cells helps immune cells differentiate between healthy and harmful microbial interactions. The T cells and antigen-presenting cells, after an antigen encounter, spur class switching of B cells. They switch B cells to more pro-inflammatory IgG classes instead of inducing IgA class switching. Activation of a type 1 response foils some bacterial infections, where inflammatory ILC3 and TH17 recruit phagocytic neutrophils. In the case of worm incursion, type 2 responses are activated. It involves ILC2 and TH2 cells, which recruit eosinophils and increase mucus production and peristalsis.
You may also like:
- Small and large intestines possess different immune system
- Intestinal Immunity can Initiate Both Type 1 and Type 2 Immune Responses
- Common intestinal diseases
- The skin immune system

I, Swagatika Sahu (author of this website), have done my master’s in Biotechnology. I have around fourteen years of experience in writing and believe that writing is a great way to share knowledge. I hope the articles on the website will help users in enhancing their intellect in Biotechnology.