In this article, I briefly describe the generation of peripheral tolerance. It refers to the mechanisms that regulate self-reactive lymphocytes after they leave the primary lymphoid organs. It ensures that immune responses against the body’s own tissues are prevented through processes such as anergy, suppression by regulatory cells, and controlled antigen presentation. These mechanisms help maintain immune balance and protect against autoimmune diseases.
Peripheral Tolerance and Immune Self-Regulation
Despite the effectiveness of central tolerance, some self-reactive lymphocytes escape deletion and enter the peripheral immune system. Mature, naïve lymphocytes capable of recognizing self-antigens are therefore occasionally present outside primary lymphoid organs. This occurs because central lymphoid tissues do not express all self-antigens during lymphocyte development, and clonal deletion requires a certain threshold of antigen affinity, which allows weakly self-reactive cells to survive.
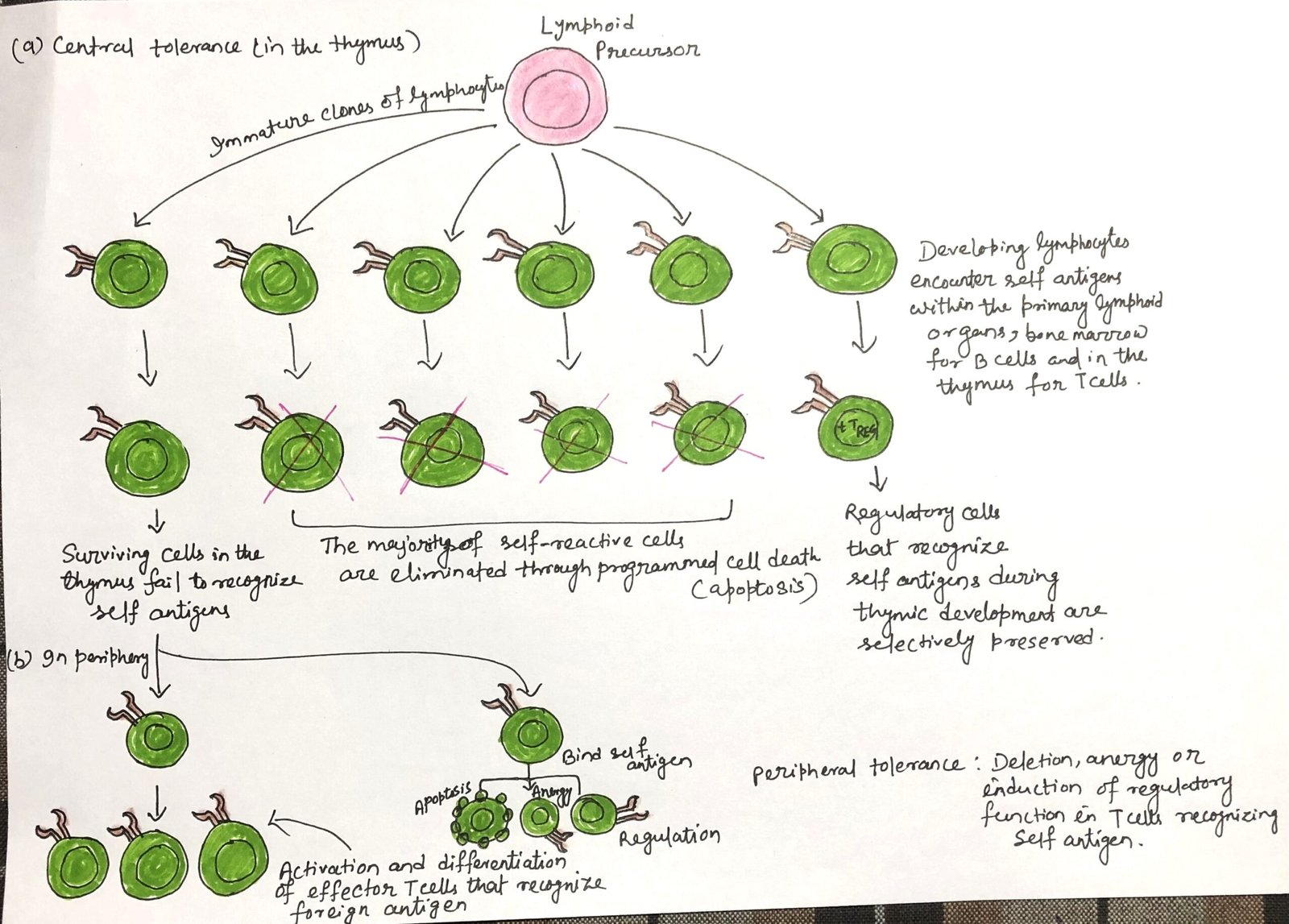
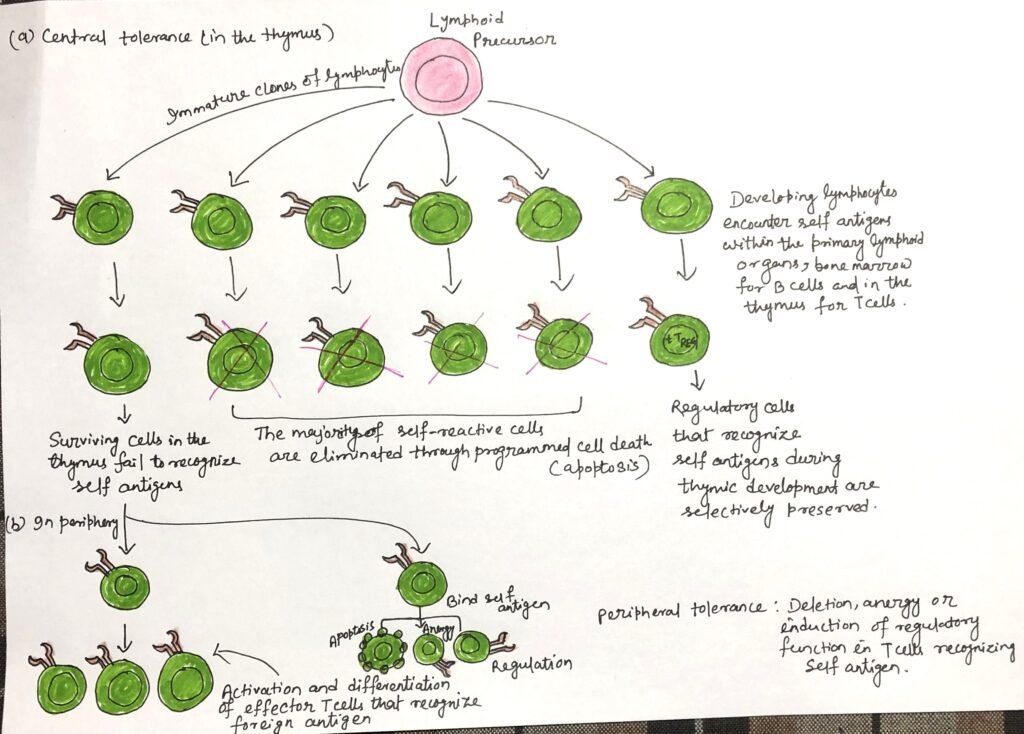
To prevent these potentially harmful lymphocytes from causing tissue damage, the immune system employs additional regulatory mechanisms collectively known as peripheral tolerance. These processes operate primarily within secondary lymphoid organs and peripheral tissues where self-antigens are encountered, ensuring immune balance and protection against autoimmune responses (Figure 1).
Mechanisms of Antigen-Induced Peripheral Tolerance
The immune system maintains peripheral tolerance through mechanisms in which mature lymphocytes interact with self-antigens and produce immunosuppression instead of immune activation. Under normal circumstances, naïve lymphocytes encounter antigens and become activated, initiating an immune response. However, antigen-presenting cells can promote immune unresponsiveness when they present antigens under particular conditions, such as specific tissue environments or regulatory signaling contexts. Scientists refer to antigens that promote this tolerant state as tolerogens, distinguishing them from immunogens, which stimulate active immune responses.
Anergy and Regulatory T Cell Induction
When a T cell encounters a tolerogen or experiences tolerance-promoting conditions during antigen exposure, it may activate pathways other than cell death. Two major outcomes are the development of anergy, where the T cell becomes functionally inactive, or differentiation into regulatory T cells. In peripheral tissues, some naïve T cells can transform into peripheral regulatory T cells (pTREGs) by expressing the transcription factor FoxP3. These cells help suppress immune activation in an antigen-specific manner.
Several factors influence the formation of regulatory T cells in the periphery, including insufficient co-stimulatory signals, inhibitory cytokines or surface molecules, and the timing and location of antigen exposure. For example, during fetal development and early neonatal life, when the immune system is not fully mature, antigen exposure often promotes immune suppression rather than activation.
Similarly, the route through which an antigen enters the body can influence immune outcomes. Some antigens administered orally can induce tolerance, whereas the same antigens delivered through skin injections may trigger an immune response. In contrast, certain mucosal antigen exposures can stimulate protective immunity, as demonstrated by the oral polio vaccine.
A key characteristic of tolerogens is their antigen specificity. The suppression they induce targets only immune responses against the specific antigen involved, rather than causing widespread immune suppression.
Factors Promoting Peripheral Immune Tolerance
In addition to fetal and early neonatal exposure, several other conditions favor the induction of immune tolerance. These include exposure to high concentrations of antigen, prolonged persistence of antigen within the body, and routes of administration such as oral or intravenous delivery. The immune system promotes tolerance when it encounters antigens in the absence of adjuvants, under conditions of weak co-stimulatory signaling, or when immature or inactive antigen-presenting cells present antigens.
The immune system further reduces the risk posed by self-reactive lymphocytes by requiring coordinated interactions among multiple immune cell types to generate a full adaptive immune response. During inflammation, effective immune activation depends on antigen presentation by activated antigen-presenting cells to naïve CD4⁺ helper T cells, which then provide signals necessary for the activation of B cells and CD8⁺ T cells recognizing the same antigen. If any of these cellular interactions are absent, incomplete, or occur in an inactive state, immune activation fails, and tolerance is more likely to develop.
Role of Regulatory Immune Cells in Peripheral Tolerance
Regulatory immune cells function primarily within secondary lymphoid organs and at sites of ongoing inflammation to control immune activity. A diverse range of immune cell types can adopt regulatory roles. Some of these cells express antigen-specific receptors, such as T-cell or B-cell receptors, that recognize self-antigens. In contrast, others contribute indirectly by supporting immune suppression through accessory functions. Despite their differences, all regulatory immune cells share the ability to dampen immune responses upon activation, acting antigen-specifically.
Although regulatory T cells represent the most extensively studied regulatory population, other immune cells also contribute to immune regulation. Distinct subsets of B cells, macrophages, and dendritic cells can acquire regulatory properties and participate in suppressing self-reactive immune responses. Together, these regulatory cell populations form a cooperative network that limits excessive immune activation and helps maintain peripheral immune tolerance.
Conclusion
Peripheral tolerance represents an essential regulatory system that ensures immune responses remain controlled after lymphocytes leave primary lymphoid organs. It operates through multiple mechanisms, including functional inactivation of self-reactive cells, generation of peripheral regulatory T cells, and suppression mediated by specialized regulatory immune cell populations. Antigen exposure conditions, co-stimulatory signals, and interactions among immune cells within peripheral tissues and secondary lymphoid organs influence these processes. While central tolerance removes many autoreactive cells during development, peripheral tolerance provides continuous surveillance and control, thereby maintaining immune stability and protecting the body from self-directed immune damage.
You may also like:

I, Swagatika Sahu (author of this website), have done my master’s in Biotechnology. I have around fourteen years of experience in writing and believe that writing is a great way to share knowledge. I hope the articles on the website will help users in enhancing their intellect in Biotechnology.