In this article, I briefly describe the working of the coinhibitory receptors CTLA-4, PD-1, and BTLA.
Coinhibitory receptor
Costimulatory and coinhibitory receptor molecules are vital in regulating immune responses to infections. Coinhibitory receptors bind with their ligands and suppress excess immune responses. When T cells get infected, they tend to express coinhibitory receptors and acquire exhausted phenotypes. They are also known as negative costimulatory receptors, which counter the activity of costimulatory receptors, thus inhibiting T-cell activation. The negative costimulatory receptors play a vital role in maintaining peripheral T-cell tolerance. They also reduce inflammation after the natural course of infection and during chronic infection responses.
The coinhibitory receptor: CTLA-4
The coinhibitory receptor cytotoxic T-lymphocyte (CTLA-4) was the first to be identified. Structurally it resembles CD28 and is also capable of binding with B7 family molecules, CD80 and CD86. The two major families of T cell co-signaling molecules are the B7-CD28 subfamily and the tumor necrosis factor superfamilies of ligands and receptors. CTLA-4 belongs to the B7-CD28 subfamily. CD80 and CD86 bind to the costimulatory receptor, CD28, and enhance TCR-mediated responses. CTLA-4 competes with CD28 for binding to CD80 and CD86, thus playing a critical role in regulating T-cell activation. Thus, CTLA-4 alienates T cell activating signals and thus, it does not act as a positive costimulator.
Rather than expressed constitutively on resting T cells, CTLA-4 expression is induced within 24 hours after activation of a naive T cell. The expression gets picked up within 2-3 days after stimulation. When compared to CD28, CTLA-4 binds with CD80 and CD86 with a higher affinity.
The expression level of CTLA-4 increases in proportion to the amount of CD28 costimulation. CTLA-4 puts a halt on the pro-proliferative influence of TCR-CD28 engagement. This is an important inhibitory function, which can be understood by the phenotype of CTLA-4 knockout mice. The T cells of these mice proliferate in an uncontrolled manner leading to lymphadenopathy, a condition of enlarged lymph nodes. This uncontrolled proliferation also leads to splenomegaly (enlarged spleen), autoimmunity, and fatality within 3-4 weeks after birth.
The coinhibitory receptor: Programmed cell death-1 (PD-1)
It is a coinhibitory receptor, also called CD279, expressed by both B cells and T cells. It has two ligands, PD-L1 and PD-L2, which are members of the Cd80/86 family. PD-L2 is expressed mainly in antigen-presenting cells. PD-L1 may mediate T-cell tolerance in non-lymphoid tissues. The interaction between PD-1 and their ligands may regulate the differentiation of regulatory T cells.
The invention of coinhibitory receptors CTLA-4 and PD-1 led to the development of checkpoint inhibitors, which act as a promising cancer immunotherapy.
Development of immune checkpoint blocking antibodies: A breakthrough in cancer treatment
Researchers have been incessantly carrying out efforts to combat cancer. Our immune system gives a frail response to tumors when compared to infection by pathogens. The multiple mechanisms of our immune system including central tolerance, regulatory T cells, and immune ignorance foil the response to tumors.
The coinhibitory receptors were developed in the 1990s and inspired many researchers to find out a possibility in cancer treatment. Dr. Jim Allison, one of the discoverers of CTLA4, thought about whether tumors use T cell co-inhibitors to evade immune attack. If cells associated with tumors or tumor cells expressed ligands for T cell coinhibitory molecules, they might be inactivating existing tumor-specific T cells. So, Allison and colleagues experimented with this possibility in mice. They injected antibodies into mice that blocked CTLA-4 interactions with tumors. Surprisingly, tumors shrunk and even disappeared.
This success led researchers to experiment on human beings. They developed a humanized antibody, which is now called ipilimumab. This antibody took time to reactivate T cells. This antibody was first tested in patients with malignant melanoma. Some of the patients respond to the treatment. It became the first cancer therapy with a survival advantage. The antibody was approved by the U.S. Food and Drug Administration for the treatment of melanoma in 2011. These therapeutic antibodies are the checkpoint antibodies that can inhibit the checkpoints in the immune system.
The working of the checkpoint inhibitor
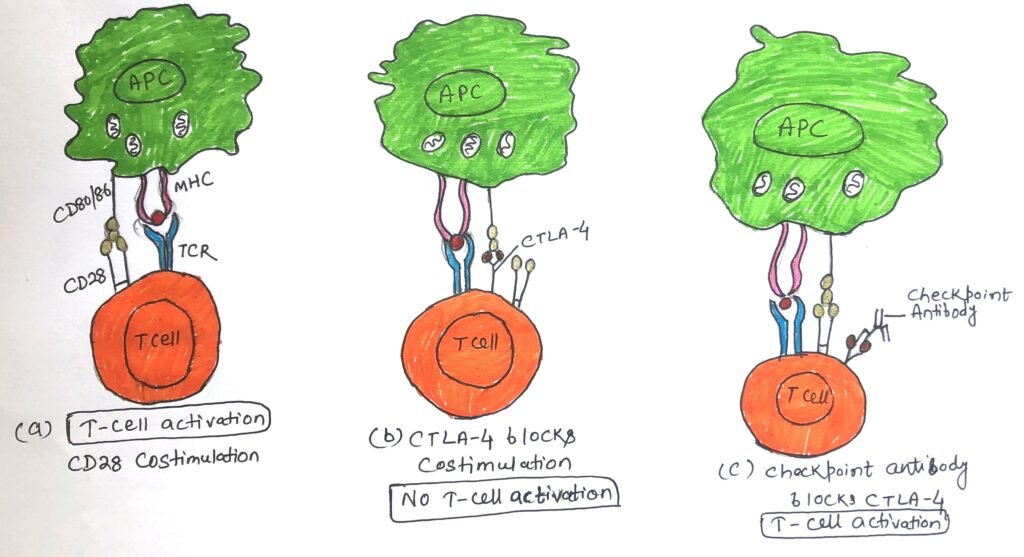
Naive T cells when engaging with both TCR and CD28 costimulatory receptors on antigen-presenting cells, get activated (figure 1a). The activated T cells increase the expression of CTLA-4, which binds with CD28 ligands (CD80/86) even more strongly than CD28 (figure 1b). This interaction between CTLA-4 and CD28 ligands inactivates the T cell. The CTLA-4 engagement with the ligands can be blocked by the antibody and thus the T cell again gains activation (figure 1c).
The Coinhibitory receptor- BTLA
The co-inhibitory receptor BTLA is also called CD272. BTLA or B and T lymphocyte attenuator is a broadly expressed coinhibitory receptor found in T helper cells, regulatory T cells, and γδ T cells. It is also expressed in NK cells, some macrophages, B cells, and dendritic cells. The primary ligand of BTLA is not a B7 family member but a TNF receptor family member known as herpes virus entry mediator (HVEM).
The expression and activity of costimulatory and coinhibitory molecules are precisely regulated
Naive T cells do not express costimulatory receptors and they get activated in secondary lymphoid tissue during the initiation of an immune response. At the end of an immune response, effector T cells up-regulate coinhibitory receptors as proliferation is not necessary. As the exploration of the genome continues, more costimulatory and coinhibitory molecules have been recognized. Knowing and understanding their regulation and function will continue to provide researchers with new tools for controlling the immune response during transplantation and disease.
Conclusion
Costimulatory and coinhibitory receptor molecules are vital in regulating immune responses to infections. Coinhibitory receptor plays a vital role in maintaining peripheral T-cell tolerance.
The coinhibitory receptor cytotoxic T-lymphocyte (CTLA-4) was the first coinhibitory receptor to be identified. It resembles CD28 and is also capable of binding with B7 family molecules, CD80 and CD86. The expression level of CTLA-4 increases in proportion to the amount of CD28 costimulation. CTLA-4 puts a halt on the pro-proliferative influence of TCR-CD28 engagement.
PD-1 or CD279 is a coinhibitory receptor expressed by both B cells and T cells. PD-1 has two ligands, PD-L1 and PD-L2, which are members of the Cd80/86 family.
The firm interaction between CTLA-4 and CD28 ligands inactivates the activated T cell. The CTLA-4 engagement with the ligands can be blocked by the checkpoint antibody, which leads to the reactivation of the T cell.
As the exploration of the genome continues, more costimulatory and coinhibitory molecules have been recognized. Knowing and understanding their regulation and function will continue to provide researchers with new tools for controlling the immune response during transplantation and disease.
You may also like:
- Costimulatory receptors for activation of T cells
- The effector cells of the immune system
- The absence of a costimulatory signal leads to clonal anergy

I, Swagatika Sahu (author of this website), have done my master’s in Biotechnology. I have around fourteen years of experience in writing and believe that writing is a great way to share knowledge. I hope the articles on the website will help users in enhancing their intellect in Biotechnology.



