In this article, I briefly describe the distribution of the normal flora in the skin, eye, and respiratory tract. Our body naturally harbors many microorganisms that live without causing harm. The skin, eyes, and respiratory tract each have their special environments where different types of normal flora thrive.
Normal Flora
The human body is home to a diverse community of microorganisms collectively known as the normal flora or microbiota. These include bacteria, fungi, and protozoa that inhabit various regions such as the skin, respiratory tract, gastrointestinal tract, and other mucosal surfaces. Among these, bacteria constitute the majority of the normal flora, while fungi and protozoa are present in much smaller numbers. Viruses, although they may persist in the body without causing disease, are generally not considered part of the normal flora. The establishment of this microbial community begins immediately after birth. At this time, the body’s external and internal surfaces are first exposed to the surrounding environment.
Skin
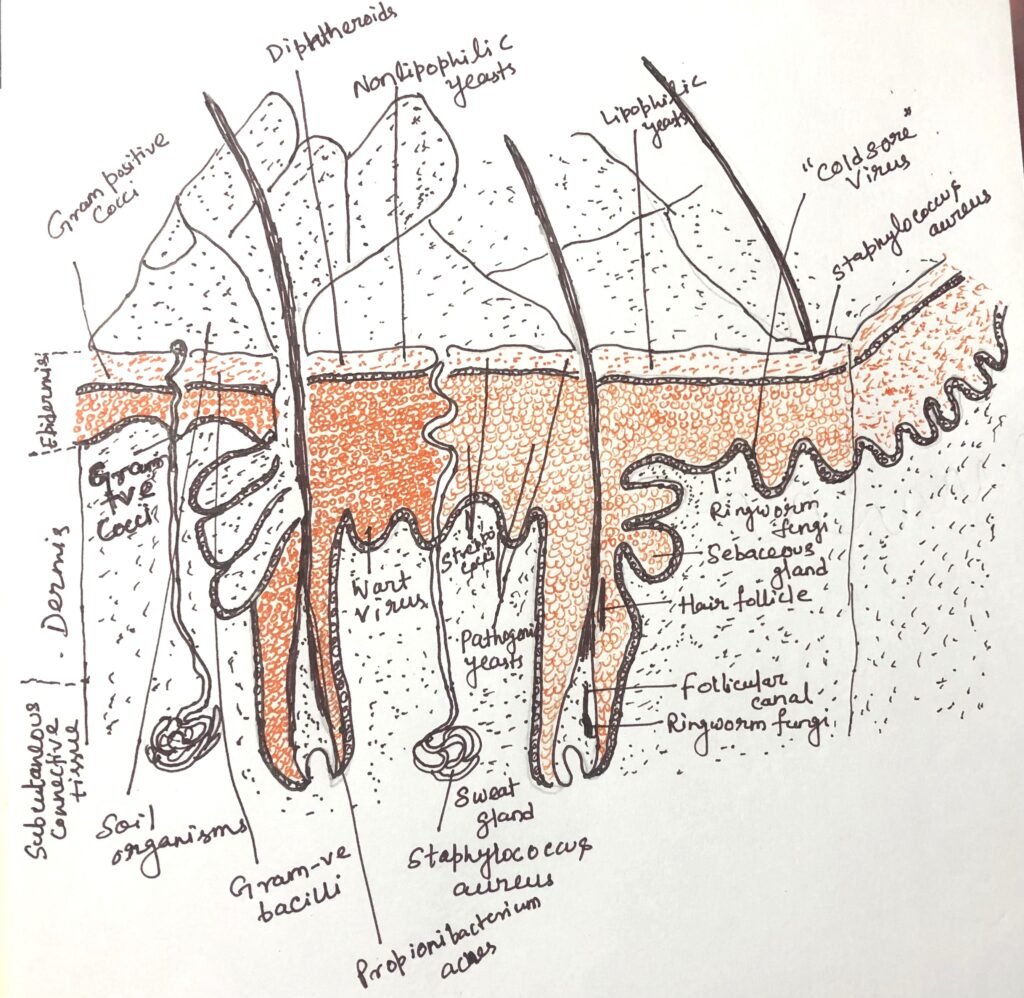
The skin consists of two main layers, the outer epidermis and the underlying dermis, which is made up of connective tissue (Figure 1). The outermost portion of the epidermis is composed of dead, anucleated, keratinized cells that form a tough protective barrier. This layer is continuously exposed to microorganisms from the surrounding environment, but is normally impermeable to bacterial invasion. However, any disruption of this barrier through cuts, abrasions, or burns can permit bacterial entry.
The structure and function of the skin vary across different regions of the body. These variations create distinct ecological niches that influence the type and number of microorganisms present at each site. Overall, the skin’s surface presents an unfavorable environment for the survival and growth of many bacteria. For example, Streptococcus pyogenes survives only for a few hours on intact skin but can persist for weeks in dry dust. Factors such as low moisture content, acidic pH, and the presence of antimicrobial substances make the skin a hostile habitat for most microbes.
Dryness of skin
The relatively dry nature of the skin restricts microbial growth. On dry surfaces, many bacteria enter a dormant state, and some may die within hours. However, certain regions of the body, such as the axilla (armpits), toe webs, and perineal area, remain more moist and thus support larger populations of normal flora compared to the drier areas.
Low pH
The skin typically maintains an acidic environment, with a pH ranging from 3 to 5. This acidity results partly from lactic acid and other organic acids produced by resident microorganisms such as Staphylococcus species. The low pH serves as a natural defense mechanism. It inhibits the growth and survival of many potentially harmful microbes that prefer neutral conditions.
Inhibitory substances
The skin also produces several antimicrobial compounds that either kill or inhibit bacterial growth. Sweat glands secrete lysozyme, an enzyme capable of breaking down bacterial cell walls. Meanwhile, sebaceous glands release complex lipid secretions, some of which are metabolized by bacteria like Propionibacterium acnes. This metabolism results in the formation of long-chain unsaturated fatty acids, such as oleic acid. This acid possesses strong bactericidal properties and helps maintain microbial balance on the skin’s surface.
The presence of strong antimicrobial defences can’t hinder the survival and multiplication of certain microorganisms. They multiply to form part of the normal skin flora. Secretions from the sweat and sebaceous glands provide essential nutrients, such as water, amino acids, urea, salts, and fatty acids, which support the growth of these microbes. The majority of the resident bacteria belong to the Staphylococcus species and aerobic corynebacteria (diphtheroids).
Within the deep sebaceous glands, lipophilic anaerobic bacteria such as Propionibacterium acnes (now Cutibacterium acnes) are commonly found. Although this organism is a harmless commensal under normal conditions, it has been implicated in the development of acne vulgaris, a common skin disorder. Because of their deep-seated location within the glands, the population of these bacteria is minimally affected by routine washing or cleansing.
Acne Vulgaris
Acne vulgaris is a disorder involving the sebaceous glands of the skin. The initial stage of the condition is marked by the formation of comedones, which occur when sebaceous glands become distended with accumulated sebum, hair, and bacteria. These comedones may remain stable or close, potentially progressing to inflammatory lesions such as papules, pustules, or nodules. This can cause visible skin disfigurement.
Propionibacterium acnes (now Cutibacterium acnes) is the predominant bacterium found in comedones. However, because it is also commonly present in normal sebaceous glands, its exact role in the pathogenesis of acne remains uncertain. Nonetheless, the observation that antibiotic therapy often leads to clinical improvement while simultaneously reducing the population of P. acnes indicates that the organism may play a significant contributory role in the development of acne vulgaris.
Eye
The conjunctiva is a thin, delicate membrane that lines the inner surface of the eyelids and covers the exposed part of the eyeball. It is constantly cleansed by the flow of tears, which helps in removing microorganisms from the surface. In addition, tears contain lysozyme, an enzyme with strong antibacterial activity. As a result, the microbial population of the conjunctiva remains sparse. The few organisms that are normally present include Staphylococcus epidermidis, Staphylococcus aureus, and Corynebacterium species.
Normal Flora of the Upper Respiratory Tract
The mucous membranes of the upper respiratory tract are more moist than the skin. However, it still provides a challenging environment for the colonization of many bacterial species. When air containing microorganisms passes through the complex nasal passages and into the nasopharynx (Figure 2), many microbes become trapped in the sticky, viscous mucus layer that coats the epithelial surface.
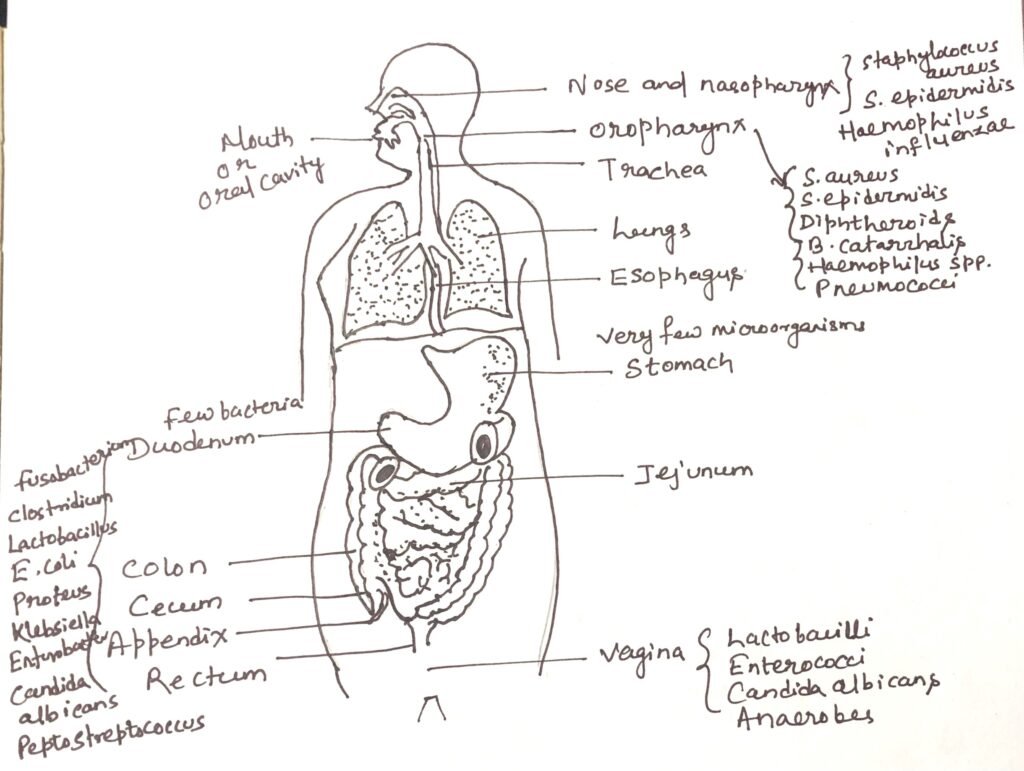
The cilia on the epithelial cells of the nasopharynx beat in a coordinated, rhythmic motion, propelling the mucus and the trapped microorganisms downward toward the oropharynx. Once swallowed, these microorganisms are usually destroyed by gastric acid in the stomach. Besides this mechanical clearance, nasal mucus also contains lysozyme, an enzyme that exerts a bactericidal effect.
Despite these protective mechanisms, the nose and nasopharynx do harbor a resident microbial flora. Their ability to persist is largely due to their capacity to adhere firmly to the epithelial surfaces. This prevents removal by mucus flow. The most common and consistent inhabitants of the nasal passages are Staphylococcus epidermidis and Staphylococcus aureus. There are also other commensal species that contribute to the microbial balance of the upper respiratory tract.
Normal Flora of the Lower Respiratory Tract
The mucous membranes of the trachea, bronchi, and bronchioles are normally free from resident microorganisms. This sterility is maintained by the continuous upward movement of mucus, propelled by the coordinated action of cilia on the epithelial cells, which effectively removes inhaled particles and bacteria.
If any microorganisms succeed in reaching the alveoli of the lungs, they are promptly engulfed and destroyed by alveolar macrophages. These are specialized phagocytic cells that form an important part of the lung’s defense system. As a result of these efficient protective mechanisms, the lower respiratory tract remains essentially sterile under healthy conditions.
Normal Flora of the Throat (Pharynx)
The throat, or pharynx, harbors a variety of microorganisms that reflect the mixed environment of both the respiratory and digestive tracts. The moist mucosal surfaces support the growth of Streptococcus species(especially Streptococcus viridans group), Neisseria, Corynebacterium, and nonpathogenic anaerobes. Occasionally, potentially pathogenic organisms such as Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis may be present as transient residents without causing disease. The balance among these microbes helps maintain a healthy microbial ecosystem and prevents colonization by harmful pathogens.
Normal Flora of the Mouth
The oral cavity provides an environment highly favorable for microbial growth because of its abundant moisture, constant supply of nutrients, and the presence of food particles. However, several natural cleansing mechanisms prevent excessive microbial accumulation. The continuous flow of saliva produces a mechanical flushing effect, carrying away many microorganisms, which are then swallowed and destroyed by gastric acid. Additionally, the shedding (desquamation) of epithelial cells helps to physically remove microbes from oral surfaces.
Despite these defenses, numerous microorganisms persist in the mouth. They possess the ability to adhere strongly to oral surfaces, such as the teeth, gums, and tongue, thereby resisting mechanical removal. These adherent species form the normal flora of the mouth, contributing to the complex and dynamic microbial ecosystem of the oral cavity.
Development of Normal Flora in the Oral Cavity
At birth, the oral cavity is essentially sterile, yet it provides a warm, moist, and nutrient-rich environment highly suitable for microbial colonization. Saliva is composed of water, amino acids, proteins, lipids, carbohydrates, and inorganic compounds. It serves as a complex medium that supports the growth of microorganisms at various oral sites.
The normal oral flora becomes established within the first few days after birth. The predominant bacterial genera include Streptococcus, Neisseria, Veillonella, Actinomyces, and Lactobacillus, along with a few yeast species. The composition of the infant’s oral microbiota depends on factors such as diet and close contact with the mother, caregivers, and environmental objects like feeding bottles and towels.
Among these microbes, Streptococcus salivarius is the most consistently isolated species, often detected as early as the second day after birth. It has a strong affinity for epithelial tissues and is found in large numbers on the dorsal surface of the tongue, marking one of the earliest and most stable colonizers of the newborn’s mouth.
Normal Flora of the Teeth
Before the eruption of teeth, most microorganisms in the oral cavity are aerobic or facultatively anaerobic species. However, with the appearance of the first teeth, conditions within the mouth change. The tissues surrounding the teeth create localized anaerobic environments. This favor the growth of obligate anaerobes such as species of the genera Bacteroides and Fusobacterium.
The tooth surface itself provides an ideal site for microbial attachment and colonization. Among the early colonizers, Streptococcus mutans is particularly significant. It is regarded as the principal causative agent of dental caries (tooth decay). This bacterium synthesizes a highly branched extracellular glucan. This acts as an adhesive “cement,” allowing bacterial cells to stick to the tooth surface and to one another. The glucan is produced from sucrose through the action of a surface enzyme called glycosyl transferase, which catalyzes the following reaction:
n Sucrose → (Glucose)n + n Fructose (Enzyme- Glycosyl transferase)
S. mutans and related streptococci ferment the fructose released from sucrose, along with other available sugars. This produces lactic acid that gradually demineralizes and erodes the tooth enamel. While S. mutans initiates the decay process, other bacteria, such as Lactobacillus and Actinomyces species, may act as secondary invaders, contributing further to the progression of dental caries.
The aggregation of bacteria and organic material on the tooth surface forms a sticky layer known as dental plaque, which harbors a dense bacterial population. Once the teeth are fully erupted, the oral flora of infants closely resembles that of adults. In addition to bacteria, some commensal protozoa may also inhabit the oral cavity. The flagellated protozoan Trichomonas tenax may reside along the gingival margins, within dental tartar, or in cavities. Its presence is more common in individuals with poor oral hygiene.
Conclusion
The human body provides a variety of habitats where different microbial communities flourish, forming the normal flora that coexist in harmony with their host. On the skin, these microorganisms adapt to varying conditions of dryness and sebum production. While in the eye, only a limited flora survives due to the constant cleansing action of tears and lysozyme. In the respiratory tract, several protective mechanisms such as mucus flow, ciliary movement, and lysozyme activity exist. However, many commensal microbes successfully colonize the nasal passages, throat, and oral cavity by adhering to mucosal surfaces. Together, these microbial populations play a vital role in maintaining the body’s ecological balance. Thus, it prevents colonization by harmful pathogens and contributing to overall health.
You may also like:
- Soil microbial flora
- Normal Flora of the Intestinal Tract
- Bacterial Exotoxins and Their Pathogenic Effects

I, Swagatika Sahu (author of this website), have done my master’s in Biotechnology. I have around fourteen years of experience in writing and believe that writing is a great way to share knowledge. I hope the articles on the website will help users in enhancing their intellect in Biotechnology.




