In this article, I briefly describe the skin immune system and its similarities and dissimilarities with the respiratory and intestinal immune systems.
Skin
The bodies of vertebrate animals are covered with a soft, flexible outer tissue layer called skin. It serves three primary roles: protection, regulation, and sensation. The skin interacts directly with the environment, acting as the body’s initial barrier against external elements. It is crucial to shield the body from pathogens and prevent excessive water loss. Additionally, the skin provides insulation, regulates temperature, senses external stimuli, and aids in producing vitamin D folates.
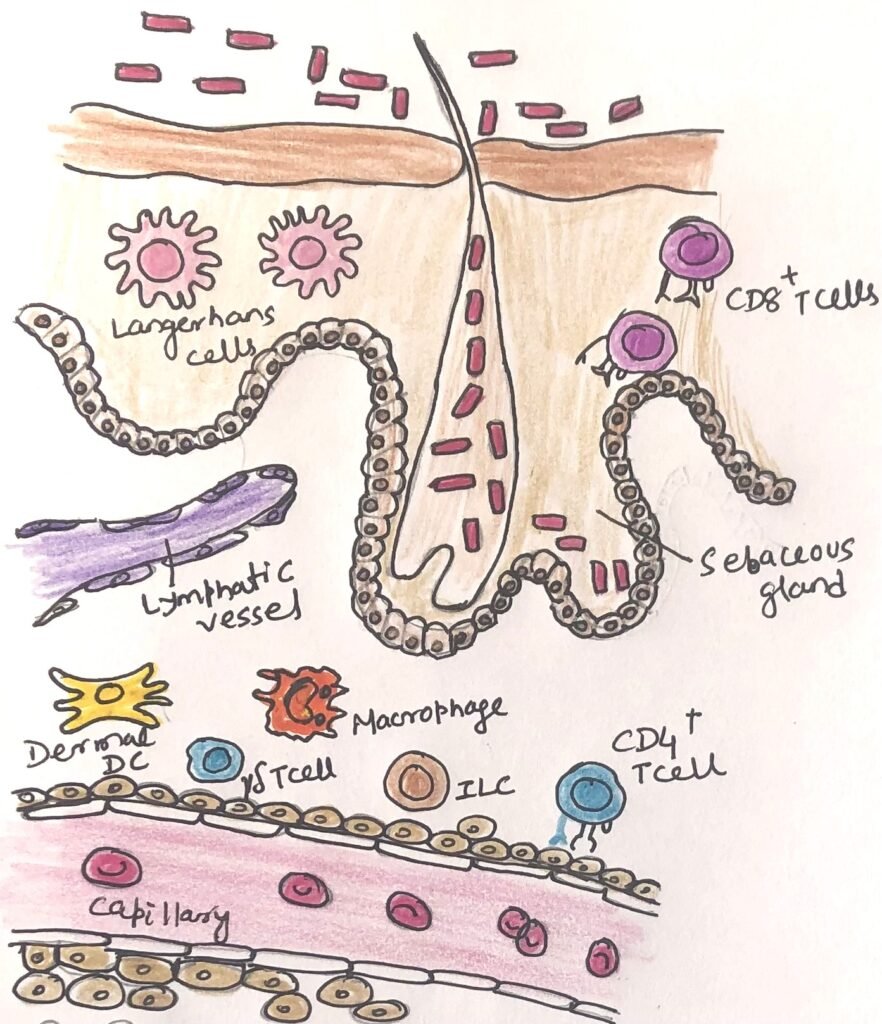
The skin is covered by multiple layers of specialized epithelial cells known as keratinocytes, which compose the epidermis. The dermis is present just underneath the epidermis. Below the dermis, the deepest layer of our skin, i.e., the hypodermis is present (figure 1). The skin epithelium is multilayered and does not produce mucus. The skin’s immune system shares many features with the respiratory and intestinal tracts.
Skin Epithelial Cells
The skin epithelial cells, also called keratinocytes, are densely packed in stratified layers in the epidermis. The new keratinocytes generated at the border between epidermis and dermis displace the layer formed by older keratinocytes. The stratum corneum forms the surface of the skin and is a 10-15µm layer of dead keratinocytes and lipids. It is a very protective, waterproof first barrier to infection. Both the skin epidermis and dermis consist of immune cells. The dermis includes hair follicles, sebaceous glands, capillaries, and nerve endings. The hypodermis is a fatty layer of arteries, veins, and sweat glands.
Skin keratinocytes not only provide a physical barrier but are active members of the innate immune system. In this way, these epithelial cells behave similarly to the epithelial cells of the intestinal and respiratory systems. Keratinocytes essentially produce antimicrobial substances and recognize pathogens through pattern recognition receptors. The specialized epithelial cells, called Langerhans cells, are found in the epidermis. Langerhans cells, along with other antigen-presenting cells, extend processes between keratinocytes. These act as sentinels that carry information about microbes from the epidermis to immune cells in the dermis. They also carry skin antigens to the draining lymph nodes. At the lymph nodes, they activate naïve T and B cells to generate immune responses. The activated Langerhans cells in the mesenteric lymph nodes can exert an influence on immune responses in other mucosal tissues.
Presence of Lymphocytes in the Skin Epidermis
Lymphocytes are also found within the epidermis and other human skin tissues, including a significant population of resident memory CD8+ T cells. While γδ T cells are plentiful in the mouse epidermis, where they extend processes similar to dendritic cells, these cells are only sparsely distributed throughout the human epidermis. The skin lacks organized lymphoid follicles, which are present in the intestine.
Most other immune cells are found just below the epithelium, i.e., in the dermis. CD8+ memory cells are the long-term residents in the epidermis, whereas CD4+ memory cells circulate in the dermis (figure 1). γδ T cells in the dermis respond to IL-23 produced by dermal antigen-presenting cells and are a primary source of IL-17 in the skin. This contributes to both protective immunity and inflammatory skin conditions, such as psoriasis. Their role in maintaining skin homeostasis is similar to that of ILC3 and TH17 cells in the gut and respiratory immune systems.
Presence of Regulatory T cells in the Dermis
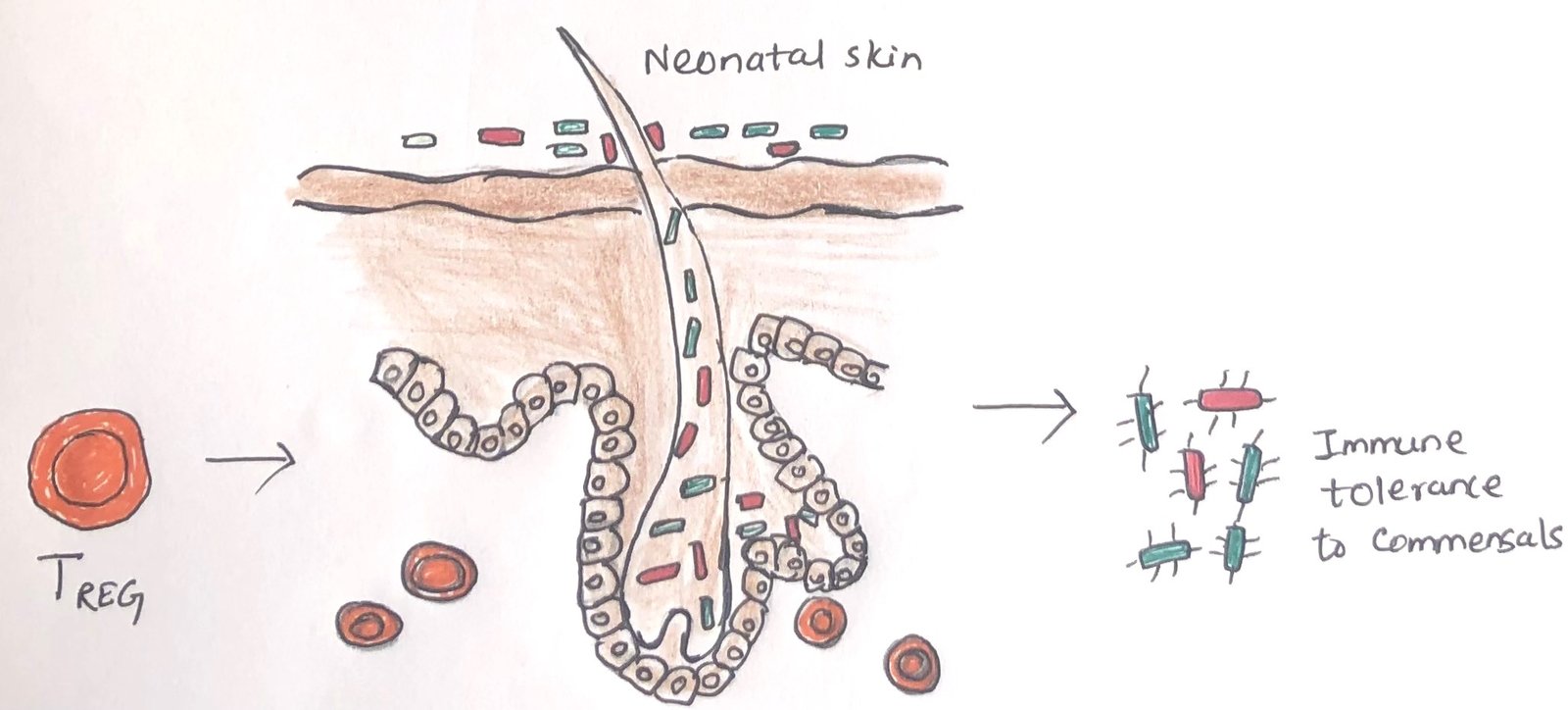
Regulatory T cells are found in plenty in the mouse and human dermis. They tend to assemble over the life span of an individual and are seen to be long-term residents. They help control tolerance to commensal bacteria and enhance inflammatory skin reactions in other barrier sites. However, according to current studies, their origin and timing of development may differ from those of intestinal and respiratory regulatory T cells.
Unlike the continuous development in response to frequent exposure to luminal antigens, as seen in the gut, regulatory T cells in the skin may be established in a single wave early in development, where they then reside long-term (Figure 2). Recent research suggests that tolerance to commensal bacteria is established within a limited period during neonatal development. For instance, studies on mice indicate that colonization with commensal bacteria only leads to the generation of tolerizing regulatory T cells if it occurs during early life; mature mice did not produce these cells under similar exposure. This finding highlights the potential long-term impact of early microbial exposure on immune health in adulthood.
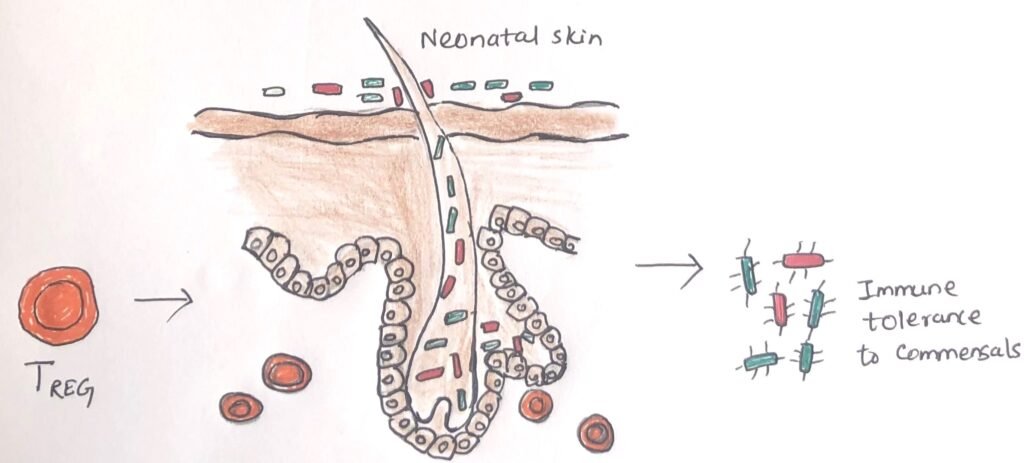
The timing of regulatory T cell development appears particularly pronounced in the skin. However, early exposure to commensal microbes and antigens likely impacts tolerance across all barrier immune systems. For instance, exposure to antigens in the lungs during the neonatal stage may help individuals avoid IgE hypersensitivities. This finding lends scientific backing to the hygiene hypothesis. According to recent research, skin TREG cells accumulate in hair follicles, which are host to commensal microbes. Commensal microbes, epithelial cells, and immune cells interact to support TREG development.
Bacteria Protecting the Skin
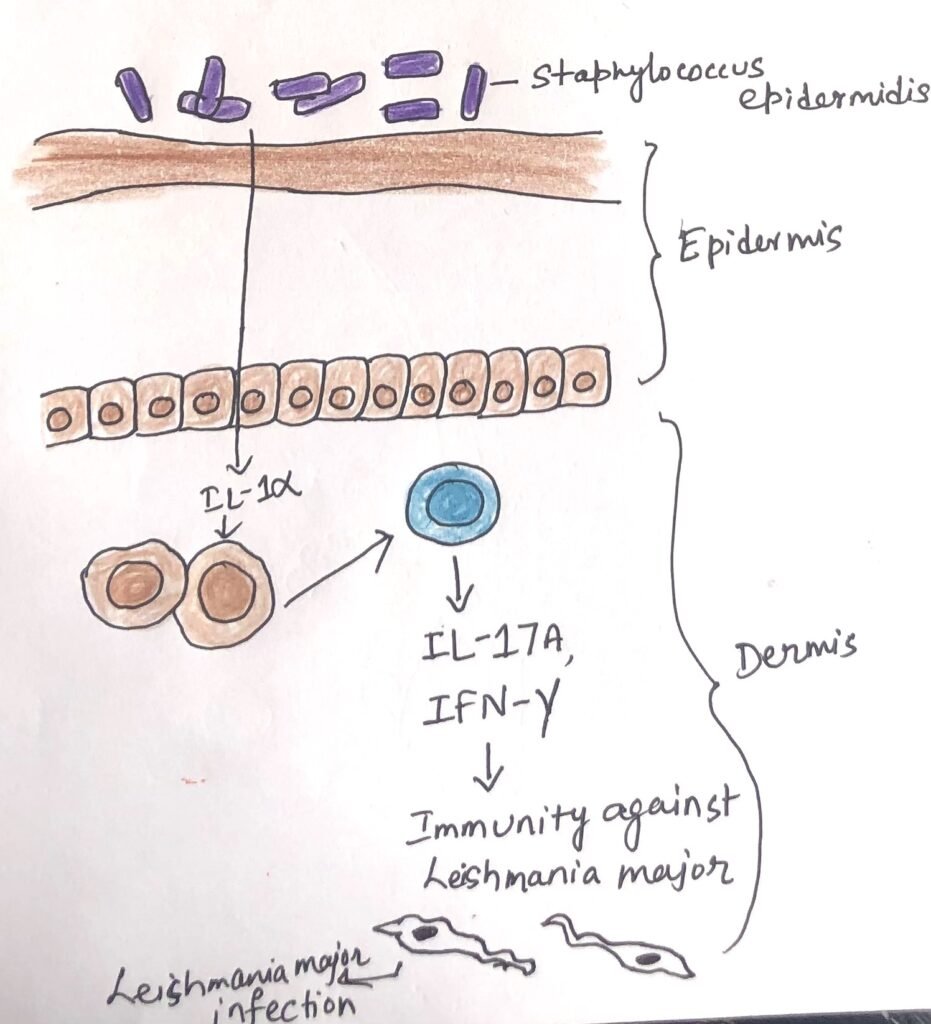
Many microorganisms, including bacteria, reside on the surface of our skin. Bacteria interact with the immune system in different ways. Specific bacterial species colonize our skin and protect us from parasite infection.
Staphylococcus epidermidis is a commensal bacterial species that interacts with pattern recognition receptors to induce the production of IL-1 by dermal dendritic cells (Figure 3). Thus, it provides protection. Production of IL-1 spurs IL-17 production by dermal CD8+ T cells, which renders a successful immune response against Leishmania parasites. Staphylococcus epidermidis induces antimicrobial peptide production by keratinocytes, thus protecting them from other bacterial infections.
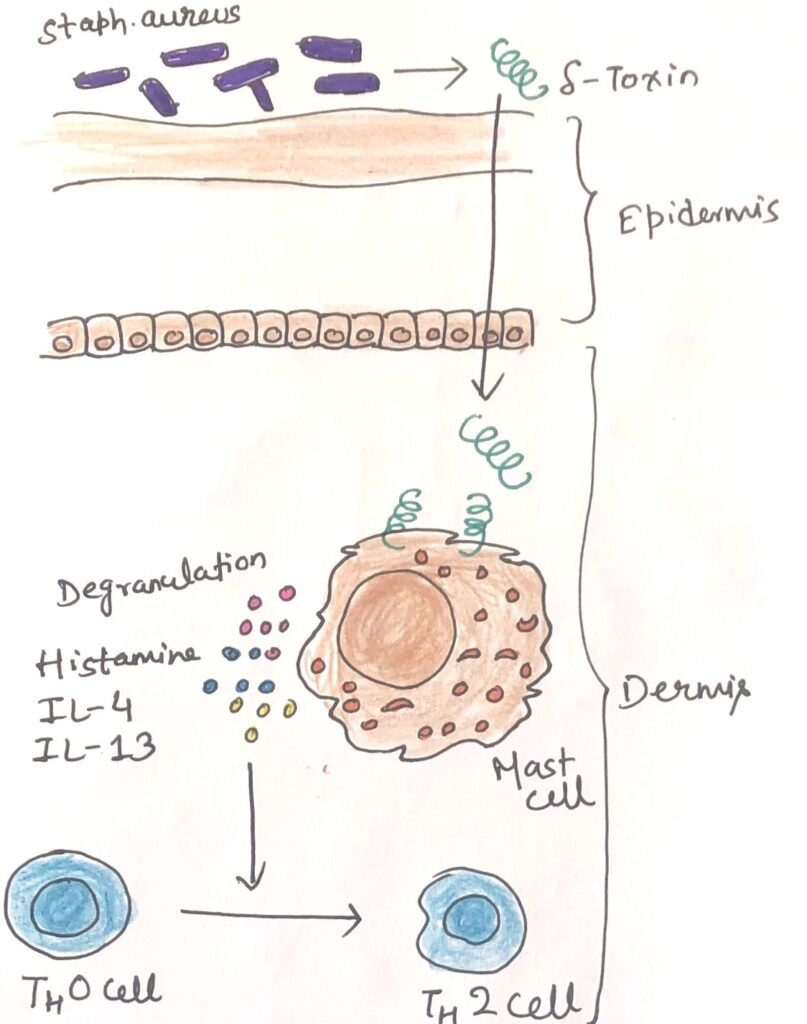
Staphylococcus aureus is the causative microorganism of allergic dermatitis. It is also associated with multiple skin and systemic disorders. S.aureus produces a molecule called δ-toxin, which penetrates the epidermal layer, thus producing inflammation. The δ-toxin interacts with dermal mast cells causing them to release cytokines that stimulate a type-2 inflammatory reaction (figure 4).
An eighteenth-century physician, Edward Jenner, was the first to identify the ability of the skin’s immune system to generate a systemic immune response along with a local response. He discovered protective immunity to smallpox, an extremely dangerous disease of humans. He did this by scratching live cowpox virus into the skin of his patients. This initiation later inspired Louis Pasteur to develop a vaccination for this fatal disease. There is ongoing research about how a local skin response triggers systemic effects.
Conclusion
The skin is covered by multiple layers of specialized epithelial cells. These specialized cells are known as keratinocytes, which compose the epidermis. Just underneath the epidermis, the dermis is present. Skin keratinocytes not only provide a physical barrier, rather are also active members of the innate immune system. In this way, these epithelial cells behave similarly to the epithelial cells of the intestinal and respiratory systems.
Lymphocytes are also found within the epidermis and other human skin tissues, including a significant population of resident memory CD8+ T cells. Most other immune cells are found just below the epithelium, i.e., in the dermis. CD8+ memory cells are the long-term residents in the epidermis, whereas CD4+ memory cells circulate in the dermis.
Regulatory T cells are found in plenty in the mouse and human dermis. They tend to assemble over the life span of an individual and are seen to be long-term residents. They help control tolerance to commensal bacteria and enhance inflammatory skin reactions in other barrier sites.
Many microorganisms, including bacteria, reside on the surface of our skin. Bacteria interact with the immune system in different ways. Specific bacterial species colonize our skin and protect us from parasite infection. Staphylococcus epidermidis is a commensal bacterial species that interacts with pattern recognition receptors to induce the production of IL-1 by dermal dendritic cells. Thus, it provides protection.
Immune responses in the skin can have systemic protective effects. An eighteenth-century physician, Edward Jenner, was the first to identify the ability of the skin’s immune system to generate a systemic immune response along with a local response.
You may also like:
- Intestinal Immunity Can Initiate Both Type 1 and Type 2 Immune Responses
- Parallelism between the intestinal immune system and the respiratory immune system

I, Swagatika Sahu (author of this website), have done my master’s in Biotechnology. I have around fourteen years of experience in writing and believe that writing is a great way to share knowledge. I hope the articles on the website will help users in enhancing their intellect in Biotechnology.