In this article, I briefly describe the type of immune responses of our intestines.
Intestine and Pathogens
Our intestinal immune system responses to specific pathogens reveal extra complexities. There are many bacteria and worms causing diseases in our bodies. Our immune system shows different types of responses to worms and bacteria. Bacteria get a type 1 immune response, whereas worms get a type 2 response from the intestinal immune system.
A Type 1 Immune Response to the Bacterium Salmonella typhimurium
There are many bacterial species causing diarrhea in vertebrates, such as Clostridium difficile, Citrobacter, Salmonella species, and E.coli. Salmonella typhimurium is a common and highly contagious bacterium that causes fever, cramps, and diarrhea in all vertebrates. Normally, the infection is cleared within a week. However, immune-compromised patients take more time to heal up completely.
Spreading of the bacterium
Salmonella typhimurium can be transferred through water, food, or feces from infected individuals. It quickly spreads and finds its way to the small and large intestines, where it can invade the epithelium.
The gut has developed multiple defenses that Salmonella must overcome to cause an infection. Initially, the bacteria must contend with the healthy community of commensal microbes and bypass defensins, the antimicrobial proteins produced by the gut lining. Certain antimicrobial peptides are especially effective at destroying Salmonella and, in some cases, can clear an intestinal infection themselves. Additionally, pre-existing IgA antibodies with broad specificity help restrict Salmonella‘s access to the epithelial barrier.
Salmonella has several alternative ways to penetrate intestinal tissue. It is frequently transported across M cells, can utilize its secretory system to invade epithelial cells, and can be engulfed by resident macrophages. During infection, Salmonella encounters the body’s next line of defense—our pattern recognition receptors. Surface toll-like receptors such as TLR4, TLR5, and TLR9 detect various antigens on this gram-negative pathogen, including lipopolysaccharide (LPS), flagellin, and CpG. Additionally, internal NOD-like receptors bind to Salmonella products and activate inflammasome responses.
Receptors respond to Salmonella
Various innate immune cells, like epithelial cells, antigen-presenting cells, and ILCs, express toll-like receptors (TLRs) and NOD-like receptors. Thus, contributing an inductive response to Salmonella. These cells cooperate and encourage a type-1 response.
Activation of pattern recognition receptors leads to the production of IL-23, a powerful cytokine that stimulates TH17 and ILC3 cells to increase IL-17 and IL-22 production. IL-22 plays a protective role by promoting the synthesis of antimicrobial proteins like REG3. Meanwhile, IL-17 boosts the production of chemokines that attract neutrophils, which are particularly effective at eliminating Salmonella. Neutrophils also release additional IL-22 and IL-17. This sequence of events, known as the IL-23-TH cell axis, helps restore the integrity of the epithelial barrier within 2 to 3 days of a Salmonella infection.
NOD-like receptors interact with pathogens and induce inflammasome activity in macrophages. It eventually activates caspase-1. Activation of caspase-1 in turn activates the cytokines IL-1β and IL-18. The cytokines IL-1β and IL-18 induce the type 1 response by inducing T-cell and ILC subsets to produce IFN-γ.
Antibodies Control Salmonella Infection
Antibodies differ in controlling Salmonella. IgA antibodies defend against the initial infection of Salmonella, whereas IgG antibodies more potently manage an active infection. Unlike IgA, IgGs are not secreted into the lumen of the intestine unless the epithelial layer is physically damaged. The IgG2a antibody is precisely effective against Salmonella infection.
Salmonella’s Defense Against Protective Responses
Salmonella has developed distinct defenses against these immune responses. It can feed on certain carbohydrates, such as sialic acid, found on proteins lining the epithelial surface. Once inside a macrophage, Salmonella exploits the acidic environment of endosomal vesicles to activate its virulence genes. It also appears to be more resistant to certain antimicrobial proteins than some commensal bacteria, and may even gain a growth advantage in their presence. Thus, a successful immune response is a race against time and a contest of evolutionary strategies between the host and the microbe.
Worm Infection Gets a Type 2 Response
Worms are highly diverse metazoans with intricate life cycles and the capability to move through various parts of our bodies. Each type of worm interacts with our immune system in distinct ways, triggering complex immune responses that offer valuable insights into our close immune relationship with microbes. Various parasitic worms infect many people. The different types of intestinal worms include hookworms, roundworms, whipworms, tapeworms, and Trichinella. The diseases they cause have symptoms, which vary from mild to severe.
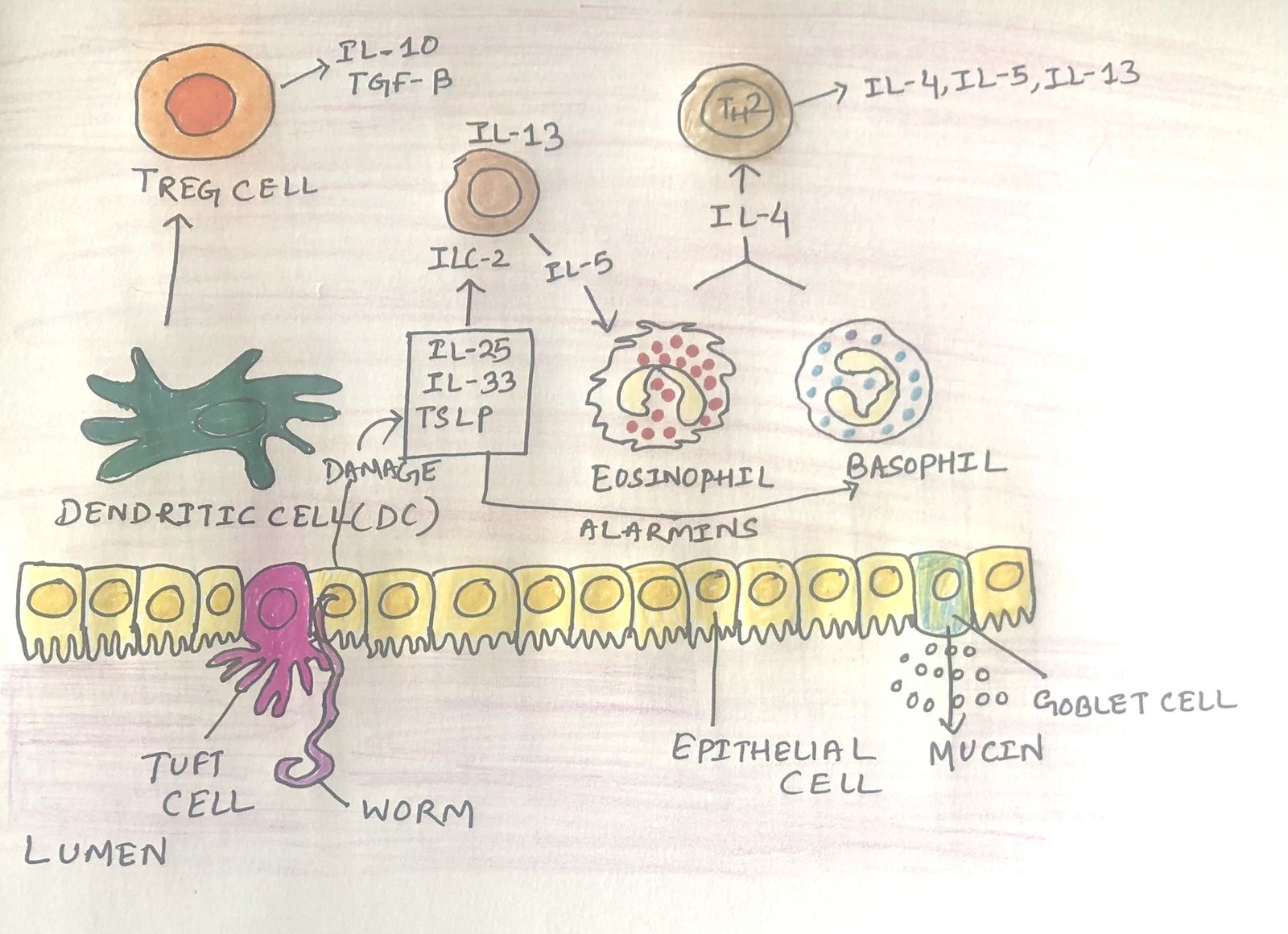
Just as our immune system has evolved alongside beneficial bacteria, it has also adapted over millions of years to coexist with intestinal worms. Some of these worms are treated as harmless symbionts, prompting tolerogenic responses that boost the production of regulatory T cells and the release of IL-10 and TGF-β cytokines. However, worms that invade our intestines encounter a highly organized defense system, shaped by our long evolutionary relationship with these organisms. Infectious worms activate a type 2 immune response, marked by the actions of ILC2 and CD4+ TH2 cells, along with the production of the typical type 2 cytokines IL-4, IL-5, and IL-13. Researchers believe that the type 2 immune response evolved primarily as a strategy to combat helminth infections (figure 1). A specific subset of cytokines, called alarmins initiate type 2 responses in the gut. These cytokines including TSLP, IL-25, and IL-33 are released by gut epithelial cells.
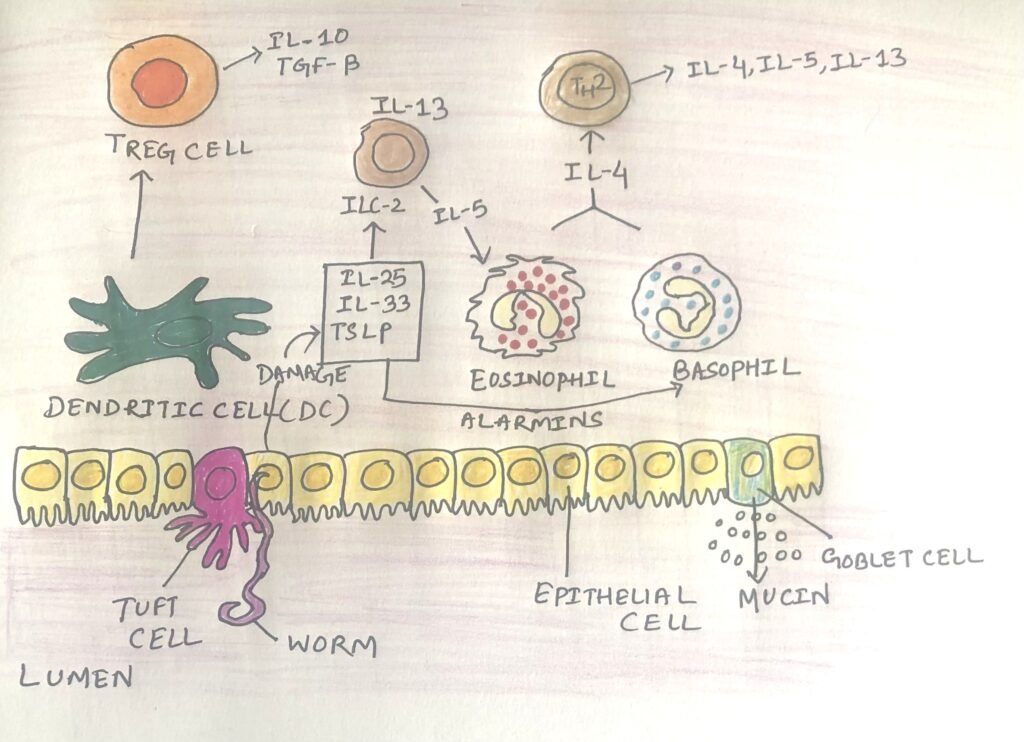
Tuft Cells Play a Vital Role in Stimulating Intestinal Cells
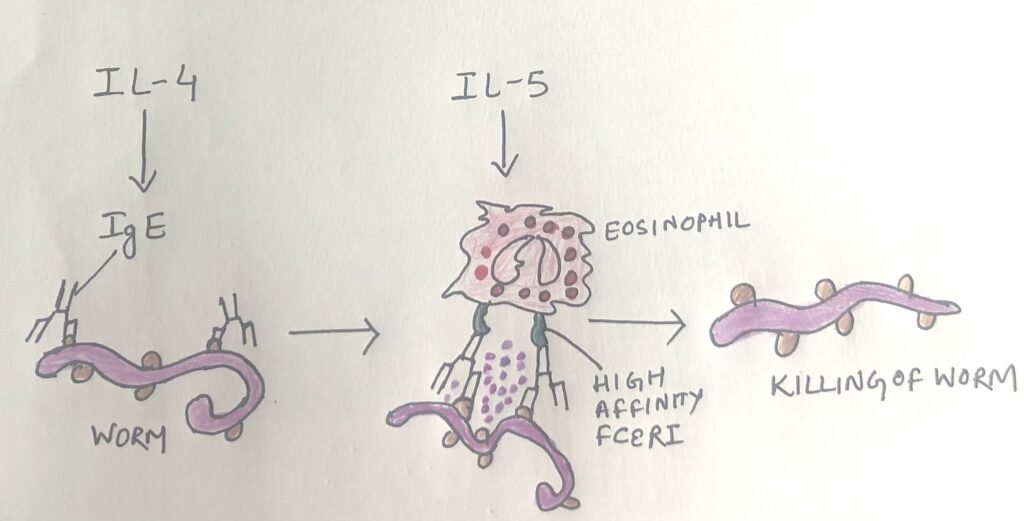
Also called brush cells, tuft cells share intriguing features with the sensory cells in the tongue that respond to umami and bitter tastes. Through their sensory receptors, tuft cells appear to detect byproducts from various parasites, including worms and protozoa. This triggers the release of alarmins and the signaling molecule IL-25, which activates ILC2 cells in the lamina propria. In response, these ILC2 cells produce the cytokines IL-4, IL-5, and IL-13. The response culminates in the production of IgE and the degranulation of eosinophils, which directly kill the worms (Figure 1).
IL-13 has a positive feedback influence on tuft cell development. It spurs the development and proliferation of more tuft cells by acting on stem cells in the intestinal epithelium. In an experiment with mice, they failed to produce enough IL-25, and thus couldn’t generate an optimal type 2 response to worms.
More Effects of Type 2 Cytokines on the Intestinal Immune System
There are multiple additional effects of type 2 cytokines on the intestinal immune system. The cytokine IL-13 increases the production of goblet cells and the secretion of mucus. This results in the clearing of worms physically from the gut. Eosinophils and basophils produce IL-4, which helps in polarizing naïve T cells to the TH2 subtype. The TH2 cells enhance the B-cell class switching to IgE.
Worm-specific IgE antibodies attach to worms through their antigen-binding sites and connect to granulocytes like eosinophils via their constant regions. This triggers the release of granule mediators, which have strong toxic effects and can be lethal to the worms (Figure 2).
Effect of Worm Exposure on the Intestine
It is thought that the increase in allergy and autoimmunity in industrial areas is due to less exposure of people to microbes. Exposure to microbes is believed to incline the immune system toward a more tolerogenic, less inflammatory state. However, ironically, worm exposure also has devastating effects on the immune system. Parasitic worms not only trigger type 2 immune responses but also promote tolerogenic reactions, which involve the generation of regulatory T cells (TREG cells) and the activity of IL-10 and TGF-β (Figure 1). The tolerogenic state has systemic consequences.
Anecdotal reports of worm exposure reducing autoimmune and allergic symptoms have led some to advocate for worm therapy. While some research supports these claims, many findings remain anecdotal, requiring further validation. Even if the approach gains traction, it’s crucial to note that regulatory T cells can impair type 1 immune responses against intracellular pathogens.
Conclusion
Our immune system shows different types of responses to worms and bacteria. Salmonella typhimurium is a common and highly contagious bacterium that causes fever, cramps, and diarrhea in all vertebrates. Certain antimicrobial peptides are especially effective at destroying Salmonella and, in some cases, can clear an intestinal infection. Additionally, pre-existing IgA antibodies with broad specificity help restrict Salmonella‘s access to the epithelial barrier.
Activation of pattern recognition receptors leads to the production of IL-23, a powerful cytokine that stimulates TH17 and ILC3 cells to increase IL-17 and IL-22 production. IL-22 plays a protective role by promoting the synthesis of antimicrobial proteins like REG3. NOD-like receptors interact with pathogens and induce inflammasome activity in macrophages. This eventually activates caspase-1.
IgA antibodies defend against the initial infection of Salmonella, whereas IgG antibodies more potently manage an active infection.
Various parasitic worms infect many people. The different types of intestinal worms include hookworms, roundworms, whipworms, tapeworms, and Trichinella. The diseases they cause have symptoms, which vary from mild to severe. Infectious worms activate a type 2 immune response, marked by the actions of ILC2 and CD4+ TH2 cells, along with the production of the typical type 2 cytokines IL-4, IL-5, and IL-13.
Exposure to microbes is thought to incline the immune system toward a more tolerogenic, less inflammatory state. Ironically, worm exposure also has devastating effects on the immune system. Parasitic worms not only trigger type 2 immune responses but also promote tolerogenic reactions.
You may also like:
- Intestinal immune system recognizes and responds to pathogens
- Small and large intestines possess different immune system
- Parallelism between the intestinal immune system and the respiratory immune system
- Type I Hypersensitivity and the Role of Genes and Environment in Allergy

I, Swagatika Sahu (author of this website), have done my master’s in Biotechnology. I have around fourteen years of experience in writing and believe that writing is a great way to share knowledge. I hope the articles on the website will help users in enhancing their intellect in Biotechnology.